If you ever ran out of toilet paper because of the COVID-19 pandemic, you may have dealt with some minor discomfort. But your health probably didn’t depend on it. Running out of medication would have been a different story. Pharmacies experienced an 8% increase in the number of active drug shortages during the first quarter of 2020. Many patients could have suffered from medication interruption due to disrupted supply chains and a 40% decline in outpatient visits from March to mid-April 2020.
Jeffrey Clement and his research team evaluated whether COVID disruptions interrupted drug therapies and in what contexts. The team analyzed 9.4 billion prescription drug claims from 252 million patients from May 2019-August 2020. They evaluated continuity of care, how many days of medication supply patients received, and the likelihood of discontinuing prescription drug therapy.
Starting in March 2020, monthly dispensing of medicines dropped significantly. About a month into COVID lockdowns, patients in most states were more likely than before COVID to discontinue hormonal contraceptives, attention-deficit/hyperactivity disorder (ADHD) treatment, antidepressants, and some antipsychotics.
These declines were concerning considering the substantial rise in anxiety and depression symptoms during the same period. For drugs used to treat ADHD, patients sometimes take summer “drug holidays” when job or school structures are more relaxed. The authors speculate that patients could have started holidays earlier in the year as work and school structures moved online or jobs were lost. Or it could have been due to an inability to reach their provider or pharmacy. In the case of antidepressants or antipsychotics, discontinuing these therapies abruptly could have led to withdrawal symptoms or worsened symptoms overall.
By contrast, patients who were using opioid addiction medications (buprenorphine/naloxone) and post-transplant drugs maintained their therapies well throughout lockdowns. The findings indicate that opioid management programs worked to manage existing patients despite the pandemic disruption. Perhaps this was because they tended to be closely managed already, and regulations were relaxed to allow for telehealth treatment. This continuity of care was crucial for patients in treatment for opioid use disorder, especially as COVID exacerbated overdose risk and mortality across the country.
Overall, there were fewer patients accessing new medications after the stay-at-home orders began, indicating COVID was more likely a barrier to starting new treatment rather than continuing existing treatment.
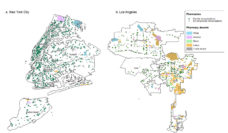
Overall, there were fewer patients accessing new medications after the stay-at-home orders began, indicating COVID was more likely a barrier to starting new treatment rather than continuing existing treatment. Community pharmacies acted quickly to facilitate access to care, with measures like free delivery of prescriptions and remote consultations. Further research could clarify if different neighborhoods experienced this access differently during COVID.
The good news? Most U.S. patients were able to access their chronic medications during the early months of COVID, especially patients in closely managed, structured programs. However, patients were still more likely to discontinue their therapies than in previous months and less likely to start new medications that may be vital to their care.
Different trends for different types of therapies suggest that a “one size fits all” model does not apply for medication continuity during crises. Novel adaptations and strategies for continuity of care will be necessary during future disruptions.
Photo via Getty Images