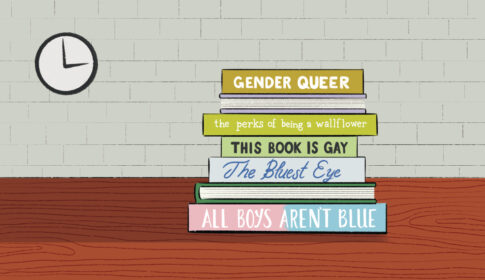
Censorship In the Classroom: Book Bans and Challenges, Part 1
PHPod sat down with Christina Dobbs, an assistant professor at Boston University Wheelock College of Education and Human Development, to discuss the current onslaught of book bans and challenges in classrooms across the country.
...more
















