Public Health Post: Generation Z seems to embrace and be more open about mental health care options than previous generations. What factors have allowed for this change in perception of mental health?
Khadijah Booth Watkins: I think there’s been more awareness and more self-advocacy, especially since COVID, when people really started to struggle. There’s also been more openness and transparency around mental health, with opportunities to talk based on what kids are seeing in schools and TV shows.
Stigma around mental health is still prevalent, but Gen Z seems more willing to explore—they don’t have the stigmatizing experiences of parents or grandparents, so they’re coming at it from a different standpoint. Even if parents or caregivers are not quite on board, teens can articulate and advocate in a way that gets them where they want to be.
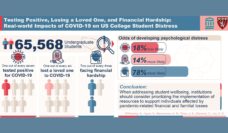
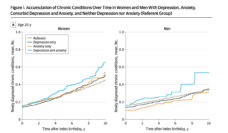
At the same time, poor mental health is on the rise, with rates of anxiety, depression, and substance use disorder increasing since the pandemic. A 2021 youth risk and behavior survey from the CDC revealed that about one-fifth of teens seriously considered attempting suicide. And Attorney General Vivek Murthy announced an epidemic of loneliness as a public health crisis. What are the greatest drivers or threats to poor mental health and loneliness among adolescents? How did we get here?
Young people are stressed in a way that they haven’t been before. It’s the many stressors, combined with an inability to engage in self-care, as well as the negative impact that social media has on those who are more vulnerable to it.
Today, kids at college don’t know if they’ll leave with job security or a fair salary. With the economic climate that we’re in, they are not so sure of their futures. And they put so much pressure on themselves to be stellar students and build up a deep resume—all these components together can be incredibly stressful. Kids also don’t make time to connect in meaningful ways with their peers.
When teens do engage socially, it is often through social media. Here, we see influencers who make their lives look so glorified and easy, and I think that is deeply misleading to a lot of kids. Comparison is the thief of joy, and it weighs on young people.
The Health Resources and Services Administration reports that the supply of adult psychiatrists is expected to decrease 20% by 2030, but demand for their services is likely to increase by at least 3%, leaving a shortage of 12,000 trained psychiatrists. This is echoed in shortages among all trained mental health professionals in the U.S. What efforts can be made to improve and increase the mental health workforce and support the growing need for these professionals?
If we put more value on mental health, I believe more people would be motivated to go into this field. Some of the drawbacks to psychiatry are financial, with concern that this specialty will not pay as much as those who went to medical school would want. More equal distribution of pay per specialty would help this.
For many providers, myself included, time spent face-to-face with patients is only a small part of care. I can bill a patient for 45 minutes, but I also speak with their parents, their school, and I write letters of support and accommodation, too. Insurance does not compensate for the collateral effort. It would help to make a more even playing field for reimbursement.
Points of affinity between providers and their patients can go a long way in supporting youth mental health, and key members of a support system, like trusted peers or family, play a very important role, as well. What key factors are needed to build resilience among students who feel less supported or who endure double and triple stigma based on their intersecting identities?
It’s important to talk to people with their strengths in mind, beyond their struggles. When we examine what loneliness looks like and the impact it has on our body, it looks the same as stress. It makes us moody and irritable and interrupts our sleep; it causes us to engage in unhealthy coping skills and strategies.
Creating an environment where kids don’t feel as alone or isolated can be a first step. I think we could best serve our patients by focusing on what makes them resilient through social support. Encouraging people, especially those with marginalized identities, to have and create meaningful connections is important to foster this sense of connectedness. I also think it’s meaningful for people to tell their story and discover strengths and resilience carefully and thoughtfully. For example, I’m a Black woman in Boston. My experience with racism and discrimination probably looks different from someone who is a Black woman in Alabama, but there might be some similarities. I think sharing stories and sharing what has helped me could help somebody else.
If you had the unlimited resources and authority to enact a single change that would disrupt the current challenges this system of behavioral and mental health care faces, what would that change look like?
I wish we could model behavioral health more like primary care—making it something that is required for your health and helps you function at your best. My one change would be to fully integrate mental health and behavioral health into overall health and wellness.
There are so many times that I hear a parent say, “if only I had known this was depression,” or “if only I had known this was ADHD.” People know the early signs of a heart attack because there was a great public health campaign to educate them and show them how to act. We must figure out how to do similar public health campaigns around mental health so people know what anxiety and depression can look like and what options and support can be available for them to seek treatment.
On December 12, Booth Watkins will speak at a Public Health Conversation hosted by Boston University School of Public Health about the challenges and opportunities surrounding college mental health. Register here.
This interview has been edited for length and clarity. Photo provided.