A year ago, social distancing, flattening the curve, and contact tracing were technical, epidemiological jargon. Now, those words are everywhere — in the news, on our social media feeds, and on road signs. Even then, it can be difficult to grasp the whirl of words and ever-changing numbers. Where do these numbers even come from? And what does testing have to do with it?
Testing 1, 2, 3 audio transcript
The Basics
With any infectious disease, an outbreak is a sudden increase in cases beyond what’s expected in a population for a certain area. A population is any well-defined group of people. It can be based on geography, relationships, or workplaces. A case is an instance of infection in a person. What counts as a case depends on the disease, the tests we have available, and the moment in an epidemic. The positivity rate is the percentage of all tests conducted that come back positive. A target positivity rate indicates whether we are testing enough to catch most cases. Reaching this target lets us know the spread is being contained.
Testing for an infectious viral disease gives us an idea of how many people are infected with a disease, the geographic regions where the disease is spreading, and how quickly. More testing is not to blame for more infections. On the contrary, testing prevents disease because it lets us know who to isolate to stop the virus from spreading to anyone else.
The Bad Beginning
At the beginning of a novel virus epidemic, we only test the people who are very likely to have the virus. Most tests come back positive and the positivity rate is high. The virus spreads, and the case number grows.
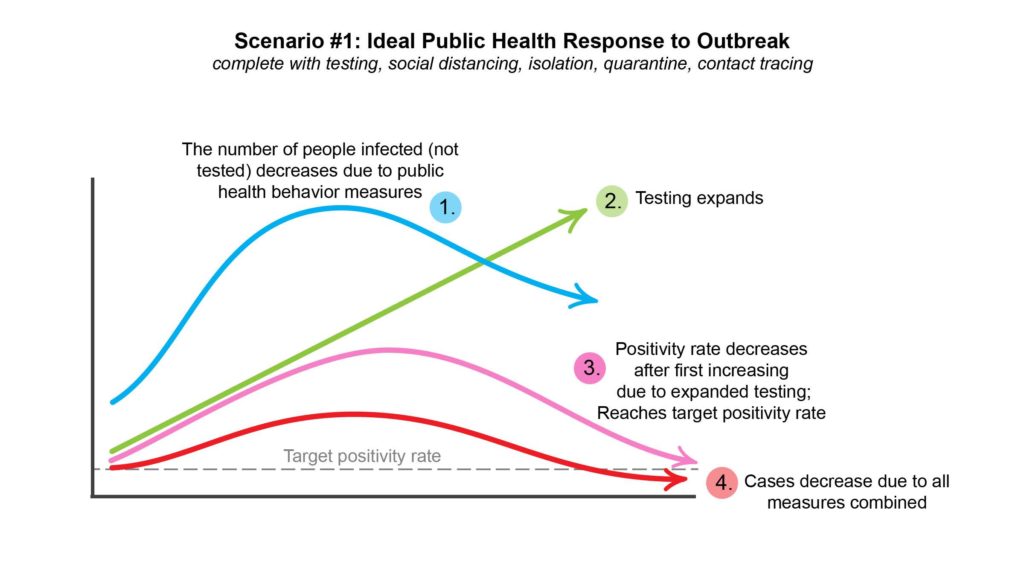
Scenario 1: Ideal Public Health Response
Ideally, populations take substantial measures – such as social distancing and contact tracing — to contain the spread of disease. At the same time, we expand testing efforts so we have a better idea of how many people are truly infected in the population. The positivity rate drops because asymptomatic people are being tested and the spread is contained. If testing and infection prevention measures are effective, cases decrease over time.
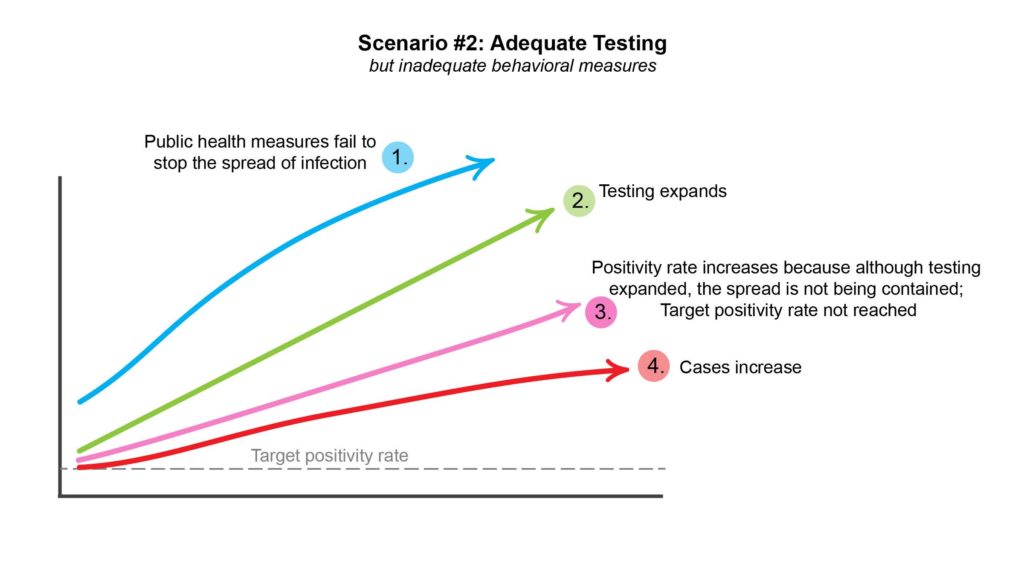
Scenario 2: Yes Testing, No Action
If testing measures are sufficient, but the population takes insufficient action to prevent new infections, then the positivity rate will not reach the established threshold. The case number will continue to rise. The epidemic is not under control.
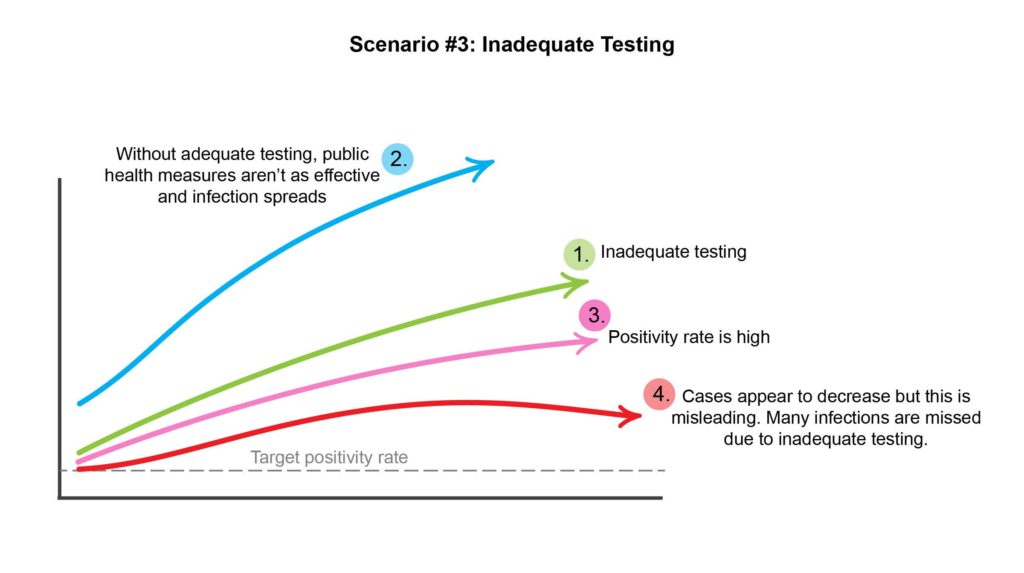
Scenario 3: No Testing, No Action
If an epidemic continues to spread quickly and there isn’t enough testing, the positivity rate is usually very high. The number of cases can appear to decrease, not because fewer people, but because we aren’t identifying them. Since cases aren’t being identified and isolated, the virus continues to spread quickly.
Testing and Action, Hand-in-Hand
It’s nearly impossible to contain the spread of a novel epidemic without reliably knowing how many people in a population are infected. The more tests being done, the more cases we identify and can act on. The more quickly we get results, the more quickly people who are infected can isolate themselves from the uninfected population.
Testing is an essential tool to contain a pandemic as we wait for a cure. To be effective, Covid-19 testing must be combined with other epidemic-stopping measures like isolation, quarantine, and contact tracing.
Data visualization by Gray Babbs and Tasha McAbee.