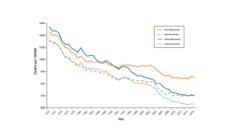
While the world tracks the battle against Covid-19 using metrics and interactive charts showing daily case counts, positive test rates, and deaths, there is another important population health measure to follow: hospital closure. Some hospitals, including those in Tennessee, Kansas, and Georgia, have closed and more are at high risk of closing. Hospital closures can be viewed as either “complete” (no health service of any kind is provided) or “converted” (inpatient units are closed, but some outpatient, emergency, or rehabilitation service is available). Since 2010, there have been 131 rural hospital closures in the United States. There is an apparent acceleration of closures with 29 urban sites in 2019, 18 rural sites in 2019, and 14 rural sites to-date in 2020. A 2016 report found one-third of rural hospitals are at risk of closing.
Individual or combined reasons for closures include a decreasing population, referral patterns excluding some hospitals, fewer services requiring inpatient stays, financial mismanagement, and disasters, such as hurricanes and flash flooding. Expansion of Medicaid under the Affordable Care Act appears to have reduced or slowed hospital closures due to improved insurance coverage and decreases in uncompensated care.
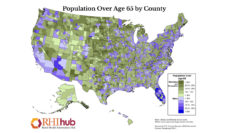
Hospital closures often have a disproportionate impact on vulnerable populations. Between 2010 and 2014, 1.5 million residents in rural areas were affected by a full or partial hospital closure. Hospitals no longer offering any health care services were more likely to occur in areas with high poverty rates. When a hospital closes, pregnant women lose access to obstetric services. Rural residents are forced to travel much further for their care.
As many hospitals and health care systems limit services and have limited operating funds in the time of Covid-19, there is a greater likelihood of more closures and a greater need to understand alternatives for increasing access to care.
An economics-based study looking at hospital closures in California found older residents reported more difficulty accessing care, decreased colon cancer screening, and a higher mortality rate for heart attacks due to travel distance to the nearest hospital. Decreased mental health and social health were reported by residents living in areas with a hospital closure. After a hospital closure, residents can feel less attached to the community, which may lead to relocation and less civic engagement.
What can be done to help alleviate the burden of care when a hospital plans to close? Strategies have involved operating a freestanding emergency department with beds for short-term observation, expanding operating hours for outpatient care, and offering telemedicine.
A number of research gaps exist. Much research relies on examination of one or a handful of hospitals making it generalization more difficult, examining consequences of care research within the past 10 years, and the effectiveness of alternative offerings to offset hospital closure has been limited.
As many hospitals and health care systems limit services and have limited operating funds in the time of Covid-19, there is a greater likelihood of more closures and a greater need to understand alternatives for increasing access to care.
Photo via Getty Images