Testing and contact tracing for Covid-19 were proposed in the early stages of the pandemic as a critical strategy to contain the spread of the virus, though the latter was never fully implemented or optimized. One challenge was that contact tracing is extremely labor intensive. For example, contact tracing for HIV in New York, one study found, costs over $500 per contact interviewed, with 85% of costs for personnel. Efforts are simpler for Covid-19, but the volume of contacts — an average of 36 per positive case — poses challenges. Nonetheless, a large labor force dedicated to Covid-19 testing has been deployed and will be required for vaccine rollout.
Workers in “nonessential” industries (such as retail and hospitality) filed for unemployment in record numbers across Canada (3 million) and the United States (20.5 million) after shelter-in-place and other preventive measures were implemented in March and April 2020. Unemployment has remained high, with rates of 9.0% for Canada and 7.9% for the US in September 2020. Many are still in need of employment, and a second pandemic wave threatens new job losses.
Expanding and extending the mandate of the public health workforce assembled for the Covid-19 response can provide meaningful employment and slow the spread of the virus. Sending health workers broadly into the community also offers a unique public health opportunity. In addition to searching for Covid-19 transmission, contact tracers could offer coordinated testing for conditions that have simple detection methods — hepatitis C virus, diabetes, and, notably, HIV — reaching populations that may not ordinarily get tested for these illnesses. While upfront investment is inevitable for all preventative approaches, offering linked HIV testing would add relatively little time to each contact and would require limited additional training, providing exceptional public health value. Achieving economies of scope in this context is no guarantee, but the potential is there.
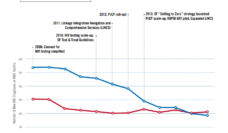
The United States’ “Ending the HIV Epidemic” strategy aims to reduce new HIV infections by 75% by 2025 and 90% by 2030. Finding and testing “hidden” cases remains difficult and testing is a weak link, even though it is well-established that it provides outstanding value and can be cost-saving in the long term. Simply learning of a new HIV infection is known to change behavior, with meta-analyses estimating an 80% reduction in sexual activity, and it can motivate newly diagnosed persons to enter into life-prolonging care.
While upfront investment is inevitable for all preventative approaches, offering linked HIV testing would add relatively little time to each contact and would require limited additional training, providing exceptional public health value.
HIV and other chronic conditions (such as diabetes) are known to disproportionately impact urban, Black and Latinx communities. Now, Covid-19 has shown the same, all-too-familiar progression. A public health workforce offering point-of-care screening for multiple conditions during the search for new Covid-19 infections could be particularly helpful to communities that experience barriers to accessing primary care.
To effectively seize this opportunity, it is imperative that ongoing testing, contact tracing, and eventually vaccination are done in a culturally competent manner that does not increase stigma and discrimination of minority populations. Stigma and lack of health care access within certain communities contribute to healthcare inequalities and are part of what contributes to HIV testing being a weak link in the Ending the HIV Epidemic strategy. Prompt linkage to community organizations that can provide mental health supports and counseling for positive diagnoses may also be prioritized in these efforts, though capacity for linkage may differ by location. Self-administered oral swabs for HIV can facilitate physical distancing and are similar in approach to most Covid-19 testing currently being conducted. Howver, point-of-care testing (including fingerstick and phlebotomy sample collection) gives immediate results, making it easier to coordinate with testing for other conditions and to facilitate linkage to care and support. As the optimal strategy would differ by community served, a best practices approach would incorporate meaningful engagement with public health personnel and community in its design.
Aside from Covid-19’s devastating death toll and contribution to loss of livelihoods, the potential long-term effects on the global economy are severe. Difficult decisions regarding how to sustain the economy most safely are already upon us. But the balance sheet can include the long-term benefits of a strengthened public health workforce that can sustain widespread HIV testing and screening for chronic diseases, reaching populations where care has historically fallen short. Although it may feel like a distant priority, the public health response to Covid-19 provides us with, as the official language of the plan goes, “an unprecedented opportunity to end the HIV epidemic in America.” Accomplishing this and expanding the impact to other health conditions is an opportunity we must not let go to waste.
The authors would like to acknowledge Laura Dale’s contribution adapting this article from the original article published in Clinical Infectious Diseases.
Photo via Getty Images