Health insurance is complicated. It’s often difficult for consumers to determine which service or provider is covered. Co-pays vary depending on what kind of clinician is seen. Patients are regularly handed shockingly large bills after hospitalizations with charges that seem unreasonable. One increasingly common surprise on medical bills is the use of an out-of-network provider, clinicians whose services insurers have decided they will not cover in full.
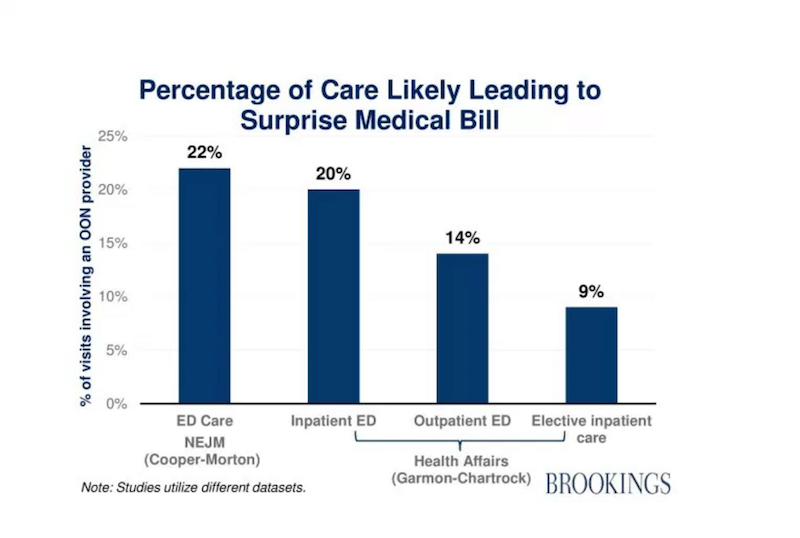
A study in Health Affairs found 9% of hospitalizations and 14% of emergency department visits result in surprise out of network charges on bills. One major reason is that even though 99.35% of visits to the emergency departments occur at in-network hospitals, about 22% of those visits include an out-of-network provider who is working there. Out-of-network providers do not have a contract with the insurer and so the charge is passed along directly to the patient. This practice is called balance billing. In these cases, the insurer will likely pay a small share and the providers then bill the patient directly for the portion not covered.
Many people do not understand the network concept or are unaware of whether their providers are in or out of network. Most patients seeking emergency services would never think to ask whether their emergency room provider is part of their insurance plan. Emergency department visits are particularly confusing as one may choose (or get driven to by ambulance without being asked) an in-network hospital but still receive a huge bill from a doctor who works there.
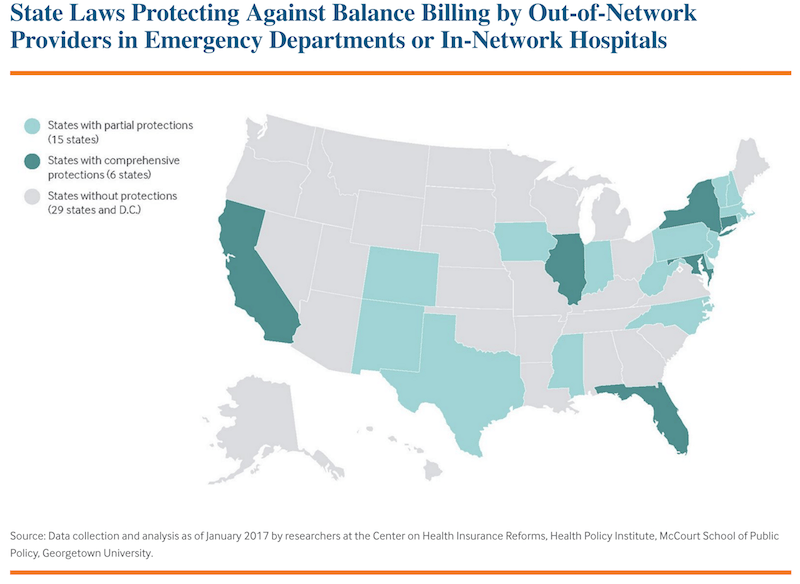
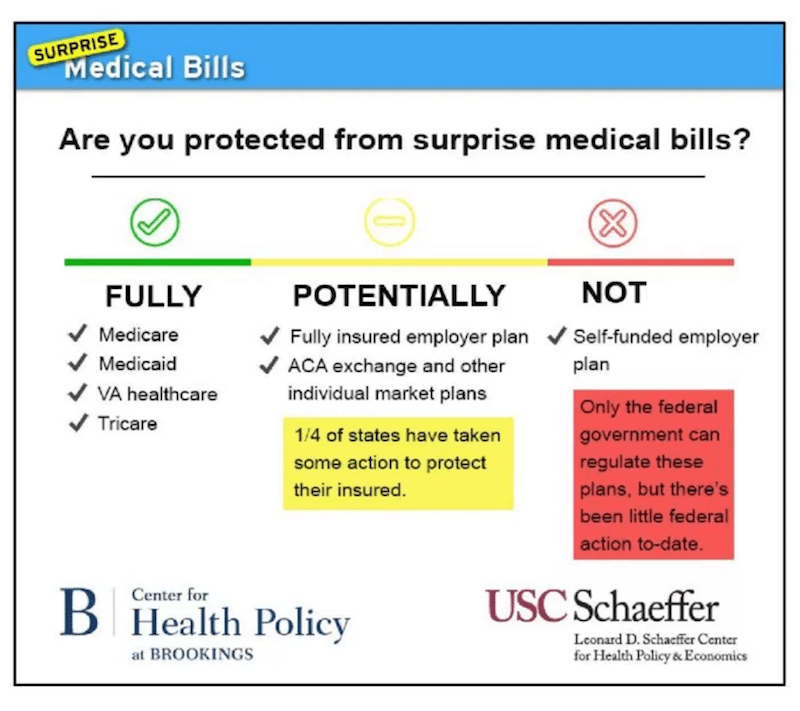
Twenty-nine states and D.C. do not have any patient protections against balance billing by out-of-network providers in emergency departments. Only six states have comprehensive protection ensuring consumers are not responsible for extra provider charges, prohibiting providers from balance billing, and requiring a discussion on a payment standard or on a dispute resolution process. States with comprehensive protections extend these to both emergency department and in-network hospitals settings. Insurers are often required to pay out-of-network providers at a certain percentage of Medicare rates. Fifteen states offer partial protection. Balance billing is just as prevalent in employer-sponsored health insurance plans as other health plans. The only comprehensive solution would be a federal policy, but this is unlikely. For now, the buyer must beware.
Feature image: urban bohemian, Medical Bills (detail), used under CC BY-NC-ND 2.0 Map from the Commonwealth Fund. Graphs from the Brookings Institute.