Over 20% of emergency department (ED) patients report food insecurity, and 18-44% report unstable housing. With a mandate to care for every patient regardless of insurance status and a longstanding commitment to caring for patients who struggle to access care in other settings, EDs are widely described as the US social and health care safety net.
Recently, new policy initiatives have encouraged health systems to systematically screen patients for health-related social needs. Programs like Accountable Health Communities have encouraged standardization of screening for social needs. To date, research on such screening practices have focused on primary care settings. Although primary care screening is important, it is insufficient because it only reaches patients with sufficient social resources to access care. Everyone else is treated in the ED.
Many ED providers express a desire to addressing social needs, but feel unable to act due to lack of time and knowledge. And, unfortunately, many EDs are ill-equipped to identify and address the health-related social needs of their patients. While individual EDs have developed screening interventions, they are often focused on just one need (e.g., food insecurity) or require significant staffing and resources (e.g., desks with volunteer undergraduates connecting patients to resources). Because of this, ED social screening at a national scale seems to be a long way off.
The goal of our study was to understand the prevalence of ED screening for health-related social needs and compare these findings to rates of screening for intimate partner violence, substance use, and mental health (common topics for ED triage screening). We conducted a cross-sectional study of all New England EDs open during 2018, asking about ED characteristics and screening practices for health-related social needs. We were particularly interested in screening to assess housing instability, food insecurity, difficulty obtaining transportation, or difficulty paying for utilities.
Because EDs are successfully screening for violence, substance use and mental health, these data suggest that social needs screening may be feasible even in busy EDs.
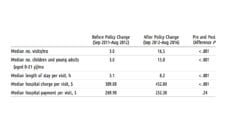
The overall response rate was 86% (166/194), and over 80% in each state. Only 39% of EDs performed any social needs screening. Thirty-three percent screened for housing instability or homelessness, 14% for food insecurity or hunger, 17% for difficulty obtaining transportation, and 6% for trouble obtaining utilities. In contrast, 95% of EDs reported screening for intimate partner violence, 89% for substance use, and 96% for mental health.
These comprehensive regional data demonstrate room for improvement in ED screening for social needs. Because EDs are successfully screening for violence, substance use and mental health, these data suggest that social needs screening may be feasible even in busy EDs. Future work for improving screening should focus on standardizing screening questions, and integrating screening data into electronic medical records.
Most importantly, we need to develop scalable strategies for responding to a positive screen and addressing the identified need. These could include a combination of community partnerships, up-to-date electronic databases of local resources and assisting patients to access resources. Together, these strategies can help us move from just identifying needs to truly helping patients address them.
Photo via Getty Images