Opioid use disorder (OUD) affects over 3 million people in the United States and continues to grow. In 2021, the number of overdose deaths exceeded 100,000, a 28.5% increase from 2020. Specifically, the overdose death rates of Black and Hispanic individuals have increased dramatically compared to White individuals. In 2020, Black individuals had the largest percentage increase in overdose deaths (48.8%) compared to White individuals (26.3%).
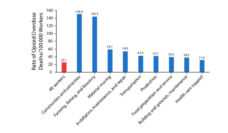
There have been comprehensive studies done about ethnic and racial disparities for OUD treatment in outpatient settings. However, little is known about these disparities for hospital-based OUD services. A study done by Jones and a team of researchers examined the relationship between the racial and ethnic composition of a community and access to OUD services in non-profit hospitals. The researchers compiled county health and demographic data of communities surrounding 613 non-profit hospitals across all 50 states to better understand the racial and ethnic make-up of the communities. They examined implementation plans for eight types of OUD treatment strategies: drug treatment, primary care, emergency services, harm reduction and education, addressing social determinants, community coalitions, prescriber guidelines, and policy advocacy. With one-in-seven hospital patients having a substance use disorder, hospitals are the perfect space for OUD interventions.
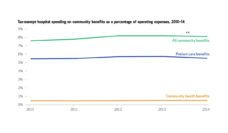
Non-profit hospitals qualify as charities to the Internal Revenue Service (IRS); therefore, they receive tax exemptions. In exchange, these hospitals are expected to meaningfully contribute to their communities. These contributions include offering free care, conducting research, and promoting community health. Drug treatment and harm-reduction services are often a part of community benefits provided by non-profit hospitals.
The strategies that were least available to Black and Hispanic communities were formal substance use treatment, harm reduction, and community coalitions which allow for culturally informed practices informed by community-specific needs.
Jones and team found that hospitals located around largely Black and Hispanic communities offered fewer OUD services than those in White communities, only about half of the services from the list of eight treatment strategies above. The strategies that were least available to Black and Hispanic communities were formal substance use treatment, harm reduction, and community coalitions which allow for culturally informed practices informed by community-specific needs.
While this study shows that the gaps in access to OUD services are present and disproportionately affect people who are Black and Hispanic, it does not suggest that hospitals aren’t responding to the needs of their communities. The researchers found that hospitals are more likely to adopt opioid-related programing in counties with greater need, as measured by the county overdose rate. Even though there is disparity in access to OUD services based on racial and ethnic make-up of communities, hospitals are partially responding to the needs of the community. Expanded Medicaid also helps with the adoption of opioid use treatment and programs.
Dr. Zoe Weinstein, an addictions researcher based at Boston Medical Center, explained her hesitations with Jones’ study saying, “Robust inpatient services that the study describes begin mostly at large academic medical centers and inpatient addiction services have really started only in the past few years. It is quite possible that repeating this study now you would have quite different findings.”
There are ways to try and shrink the racial gap in addiction services. Harm reduction programs can be effective in reaching racial/ethnic minority patients and center around empowerment, pragmatism, and goals for moderation. In areas with lower hospital-based OUD service interaction, community coalition work could greatly improve the uptake of available OUD services. Another way is to continue to support Medicaid expansion. Increased financing of Medicaid results in more opioid treatment programs. Dr. Weinstein explains, “We need to build anti-racist, culturally appropriate care—inpatient and out. One step is to have an addiction workforce that reflects the communities we want to serve. We need to reach out and meet people where they are.”
Photo via Getty Images