Is a prescription worth the paper it’s written on if you can’t afford to fill it? This is a question unfortunately faced by many Americans. Cost-related nonadherence, or CRN, describes this situation, when patients cannot follow through on the recommendations of their doctors because of prohibitive medication costs. Although the majority of these individuals tend to be uninsured, many people with both private and government health coverage still find themselves struggling to pay for the medicine they need.
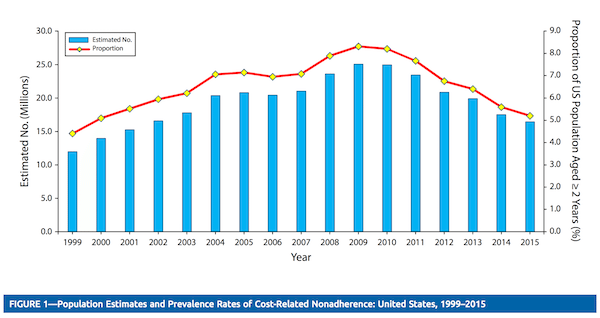 A study published in October by Joe Kennedy, PhD and Elizabeth Beth Geneva Wood, MPHA points to how recent policy changes may have affected the rate of CRN among adults and children in the US. Kennedy and Wood used data from the National Health Interview Survey to examine trends among seniors, adults and children from 1999 through 2015. Any case in which a survey respondent reported skipping or delaying filling a prescription or taking less medicine than prescribed in order to save money was counted as an episode of CRN. This timeframe covered three important events for many people’s ability to pay for the medication they need: the passage of the Medicare Modernization Act of 2003, the beginning Great Recession in 2008, and the passage of the Affordable Care Act in 2010.
A study published in October by Joe Kennedy, PhD and Elizabeth Beth Geneva Wood, MPHA points to how recent policy changes may have affected the rate of CRN among adults and children in the US. Kennedy and Wood used data from the National Health Interview Survey to examine trends among seniors, adults and children from 1999 through 2015. Any case in which a survey respondent reported skipping or delaying filling a prescription or taking less medicine than prescribed in order to save money was counted as an episode of CRN. This timeframe covered three important events for many people’s ability to pay for the medication they need: the passage of the Medicare Modernization Act of 2003, the beginning Great Recession in 2008, and the passage of the Affordable Care Act in 2010.
According to the study, the overall rate of CRN in the U.S. rose steadily at the outset of this period, from just over 4% of the population to 8.3% in 2009. The researchers observed that this peak corresponds with the height of the Great Recession. There was one notable exception to this trend. The CRN percentage for adults over the age of 65 peaked at 5.4% in 2004 before falling to 3.6% in 2006, coinciding with the full implementation of Medicare Part D.
Any case in which a survey respondent reported skipping or delaying filling a prescription or taking less medicine than prescribed in order to save money was counted as an episode of CRN.
While this rate rose again for seniors between 2007 and 2010, also likely tied to the recession, CRN has consistently been a much more prevalent problem among working-aged adults. At the peak of the economic downturn 2009, an estimated 21 million adults ages 19-24, or 11.3% of the US population, reported being unable to afford to fill a prescription. These numbers fell slightly as economic conditions began to improve after 2010, to 11.1%. However, one group in particular saw much more dramatic gains: young adults between 19 and 25 years old. Between 2010 and 2011, when the ACA provision allowing young adults went into effect, this group saw a reduction in CRN from 10.8% to 8.2%.
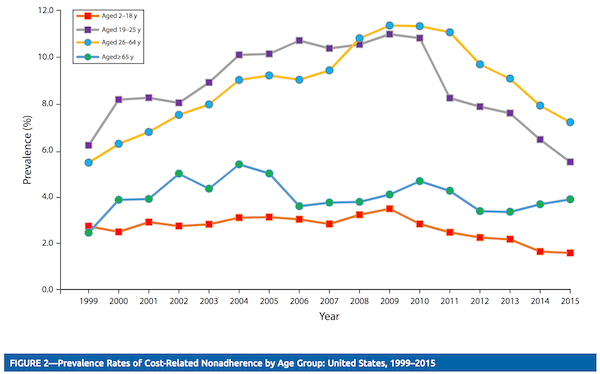 Steeper reductions began to be seen as other parts of the ACA such as health insurance marketplaces and, in some states, expanded Medicaid coverage came into effect in 2014. By 2015, the total percentage of adults who reported an episode of CRN in the previous year fell from the aforementioned 11.3% in 2013 to 9.1%, a reduction of about 4.5 million people.
Steeper reductions began to be seen as other parts of the ACA such as health insurance marketplaces and, in some states, expanded Medicaid coverage came into effect in 2014. By 2015, the total percentage of adults who reported an episode of CRN in the previous year fell from the aforementioned 11.3% in 2013 to 9.1%, a reduction of about 4.5 million people.
While the authors of this study state that their results cannot be taken as conclusive evidence that the ACA has directly impacted the prevalence of Cost-related non-adherence in the US, they do strongly suggest that certain policies has an impact on whether people are able to afford the medications that they need. This research, along with others that examine the potential gains made under the ACA, need to be carefully considered as policymakers, especially Republicans on Capitol Hill, consider the making widespread changes national healthcare policy.
Feature image: Derek Gavey, Bad Drugs, used under CC BY license/cropped from original
Graphs from Medication Costs and Adherence of Treatment Before and After the Affordable Care Act: 1999–2015, Jae Kennedy, PhD, and Elizabeth Geneva Wood, MHPA.