Obesity is an immense public health challenge in the US. The prevalence of obesity in adults increased by 30 percent between 1999–2000 and 2015–2016. Currently, 40 percent of adults are living with obesity. By 2030, close to half of adults will be living with obesity, putting them at increased risk for illness and disease. How we respond to the obesity crisis depends on what we think the risk factors are. Mounting evidence suggests that stress is a key risk factor to obesity.
Exposure to social and environmental demands (often referred to as stressors) can have behavioral and physiological consequences that increase the risk of obesity. Psychosocial stressors, such as exposure to discrimination, childhood trauma, and relationship conflicts are associated with weight gain. To date, however, most studies have focused on one stressor, which severely underestimates the true impact of stress in the development of obesity. Stress is multidimensional and people experience multiple psychosocial stressors simultaneously.
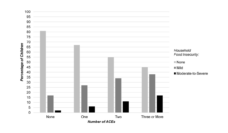
The interdisciplinary Psychosocial Determinants of Health Group (PSDH), which I lead, used secondary data from the Chicago Community Adult Health Study, to quantify the associations between obesity and eight psychosocial stressors: childhood adversity, acute life events, financial strain, neighborhood stressors, employment stressors, job discrimination, relationship conflict, and discrimination. We found that childhood adversity, acute life events, financial strain, and relationship stressors were associated with increased odds of obesity. Participants who reported experiencing many of these stressors frequently and simultaneously had even greater odds.
Non-Hispanic Black and Hispanic adults suffer from higher rates of obesity compared to non-Hispanic White adults. Non-Hispanic Black and Hispanic adults also report experiencing greater exposure to common and race-related stressors such as financial strain and racial discrimination. Building on our findings, we set out to examine whether exposure to an accumulation of stressors helps explain racial/ethnic differences in obesity disparities. To do this, we quantified the individual and joint contribution of obesity-related risk factors, including physical activity, fruit and vegetable intake, socioeconomic position, and stress exposure.
Our findings suggest that multiple types of stressors may be risk factors for obesity, and cumulative exposure to these stressors may contribute to obesity and obesity disparities.
We found that, together, all the risk factors explained less than 20 percent of differences between any racial/ethnic minority group and White individuals. Socioeconomic position and health behaviors did not explain obesity differences between racial/ethnic minorities and White individuals. High levels of stress in four or more domains explained 4.46 percent of the differences between Black and White individuals. And high levels of stress in three domains significantly explained 14.13 percent of differences between US-born Hispanic and White.
Our findings suggest that multiple types of stressors may be risk factors for obesity, and cumulative exposure to these stressors may contribute to obesity and obesity disparities. Individuals who are obese may be exposed to more psychosocial stressors than individuals who are normal weight. Compelling evidence shows that people with obesity experience discrimination and other social problems in society. Other obesity-related risk factors need to be examined to understand the underlying mechanisms explaining these disparities. Our findings can be used to inform policies and interventions addressing obesity and obesity disparities.
Stress management has received little attention at the national or state level. In fact, only 40 percent of mayoral officials identified stress as having a very strong effect on health disparities. Stronger political will is needed to address stress and obesity at the policy-level. Programs that build social capital (e.g., neighborhood cohesion and social support) in marginalized communities can redress the causes and consequences of obesity.
Photo via Getty Images