Approximately 40% of all unpaid family caregivers in the United States are men (16 million), and this percentage has been consistently increasing. Men’s contributions to long-term caregiving have been marginalized and under-estimated, especially when some do not label themselves as caregivers despite performing tasks that would characterize them as such and, instead, identify as a relative of the care recipient, such as husbands tending for their wives.
Using the 2011 and 2015 National Study of Caregiving (NSOC), we studied the emotional, financial, and physical burden of men who are spouses or partners, sons and other caregivers. For each sub-group, we assessed the impact of personal characteristics, caregiving tasks, and supportive resources. Previous scholarship has mostly studied female caregivers, one type of male caregiver, or small non-random samples. We contribute to the existing literature by studying two years of a nationally representative dataset, by focusing only on men as caregivers and on their relationship with the care recipient.
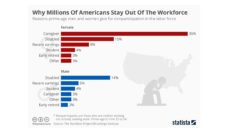
Our findings highlight that men are not a monolithic group behaving homogeneously and experiencing caregiving in the same way. Gender is only one facet of a caregiver’s identity. Combined with other factors and roles, gender affects caregiving style, tasks, and experience. Like women, men face caregiving burdens but have weaker support networks and are less likely to seek out programs that help them cope with this strain.
All male caregivers experienced emotional, financial, and physical burdens and vastly underutilized support and training services. But their reported levels of emotional stress were particularly high. Sons had the highest emotional and financial strain levels despite accessing the greatest amount of resources, including caregiving training and information.
We need to pay attention to caregiver wellbeing because they significantly contribute to societal welfare. If it takes a village to raise a child, it takes an entire country to support our loved ones, care recipients, and caregivers.
Assisting with personal care activities (especially bathing) was the most stressful task. In fact, personal care assistance is considered to be the most difficult task by all caregivers regardless of gender. Despite this burden and discomfort, men are increasingly performing complex personal care and medical tasks such as giving injections, tube feedings, catheter care, and interacting with providers, agencies, and professionals as advocates for their care recipients.
Our results also suggest that caregiving burden lightens with help from family and friends. Having time to decompress and feeling appreciated by the care recipient were also beneficial. In fact, feeling appreciated by the care recipient was always linked with lower odds of all three burdens and 88% of our sample felt appreciated by their loved ones.
Most research on family caregiving has historically focused on female assistance, so existing policies supporting caregivers are aimed at women and how they care for a loved one. But researchers acknowledge significant differences in caring patterns, burden, and responses to caregiving between men and women caregivers. For example, male caregivers may sometimes have a more task-oriented approach to care and access fewer formal services, whereas female caregivers may use more emotion-oriented coping methods. Our findings offer insight for devising future caregiving policies which explicitly acknowledge gender, relationship, and burden type differences that support and prepare men to embrace this important role without compromising their wellbeing.
No caregiver, man or woman, can undertake such an intensive task alone. We need to pay attention to caregiver wellbeing because they significantly contribute to societal welfare. If it takes a village to raise a child, it takes an entire country to support our loved ones, care recipients, and caregivers.
Photo by Mariah Ashby on Unsplash