Every few months I grit my teeth for an HIV test. My doctor made it part of my routine labs after I confessed that I hadn’t been tested in several years. Status awareness is now a key part of efforts to reduce the spread of HIV.
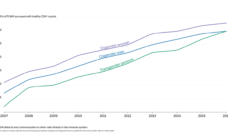
At the start of the HIV epidemic, 100,777 deaths due to AIDS were reported in the first ten years. The LGBT+ community came together and rose to the challenge of fighting the disease and the stigma that came with it.
In 2020, almost 31,000 people received an HIV diagnosis in the U.S., a number far lower than decades earlier. By knowing their status, people took steps to prevent spreading or being infected with HIV.
The CDC recommends that all people over 30 be tested for HIV at least once. Men who have sex with men and people who inject drugs are considered higher risk and should be tested annually. However, less than 30% of high risk people in the U.S. have ever been tested. Research suggests that stigma around HIV diagnosis plays a key role in dissuading people from testing.
Stigma is a social process usually characterized by stereotyping, labeling, or discrimination based on a feature or trait perceived to be a disadvantage. Stigma creates negative attitudes and beliefs towards people. Sometimes stigma can be internalized and create a reluctance to seek help or treatment. Surveys in recent years found that 17.5% of adults and over 30% of adolescents feared casual contact with HIV positive people. This suggests that stigma against people living with HIV continues in the U.S. despite more than thirty years of progress in treatment, prevention, and testing.
According to the CDC, 13% of people with HIV do not know they are infected.
To assess the impact of stigma on HIV testing, Bradley Lott and fellow researchers conducted nine focus groups with 64 men who have sex with men (MSM) in Detroit. The focus group discussion questions focused on HIV, stigma, and HIV testing. The study included Detroit area MSM of varying ages, races, and some who were HIV positive.
A 2018 survey reported that over 10% of LGBT people have had a healthcare provider refuse to see them due to sexual orientation. This number increases to almost 30% of transgender people surveyed. A focus group member in the Detroit study was turned away from emergency rooms when seeking post-exposure treatment to prevent HIV. Others were denied STI testing by private practitioners.
Black participants reported the stress of rejection more frequently than White focus group members. They feared refusal of care by healthcare providers, and also rejection by friends and family. Some reported that if they were seen at a clinic that tested for HIV, people would assume they were HIV positive. The fear of being rejected is likely associated with why some did not receive regular testing for HIV.
According to the CDC, 13% of people with HIV do not know they are infected. The researchers suggest making HIV testing more routine. Along these lines, it may be more feasible to have physicians simply, discuss HIV risk behaviors during regular visits and offer testing routinely rather than testing routinely. This could reduce stigma without overburdening people with testing if they are not at risk.
It’s been over 40 years since the first case of HIV in the U.S. We’ve improved testing and treatment options, yet social stigma around HIV still isolates people today and can prevent them from being tested. I am fortunate enough to have a doctor who doesn’t shy away from discussing HIV with me. We treat it as we would any other health risk.
Photo via Getty Images