Recent reports indicate troubling declines in the health of rural Americans and a growing rural-urban mortality disparity. Rural areas are further constrained by provider shortages and a rural hospital closure crisis. Accordingly, rural populations may engage differently with the health care system, particularly for acute, unscheduled care needs increasingly seen in emergency departments (ED). ED use patterns provide a lens into health care delivery within the community they serve. As emergency physicians and health policy researchers, we believe EDs may be increasingly caring for rural patients in ways distinct from the urban experience. We investigated health care use trends of rural populations to gain insights into rural health disparities.
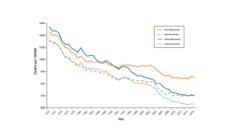
Using the most recent 12-year period (2005-2016) of the National Health Ambulatory Medical Care Survey, we evaluated changing trends in rural and urban ED visits. We wanted to see if changing patient demographics and insurance coverage contributed to these trends. We also looked at the acuity of ED visits and whether they were for medical problems tied to poorer quality outpatient health care—also called ambulatory care sensitive conditions. Finally, we examined the proportion of EDs that meet safety-net classifications, defined as those heavily reliant on public insurance, which can contribute to eroding financial solvency of rural hospitals.
We found a substantial increase in patient visits between 2005 to 2016 in rural EDs–growth of over 50%–despite an overall decline in the US rural population. Our data indicate that, by 2016, nearly one-fifth of all ED visits occurred in rural settings. This uptick in ED use was particularly high among adults age 18 to 64, non-Hispanic Whites, Medicaid recipients, and the uninsured. We also found that rural EDs were increasingly serving as safety-net providers for an increasing number of Medicaid patients and a steady number of uninsured. This is in contrast to the urban ED experience where uninsured visits declined while Medicaid visits rose–indicating a likely shift in insurance status for urban dwellers not seen in the rural setting.
Rural health faces many barriers, but we already see rural-centric innovation born from challenges to improve rural health.
The disproportionate rise in rural ED visits, particularly for vulnerable populations, suggests several considerations for rural health. Increased visits by young-to-middle aged White rural patients–particularly those receiving Medicaid or uninsured–may indicate increased burden of illness or challenges in accessing other sources of care. Further, rural patients may face barriers to timely outpatient ambulatory and primary care services as evidenced by increased ED visits for conditions that are potentially prevented or treated.
Finally, increased dependence on Medicaid reimbursement may give an important boost to rural hospital financial stability. Recent analyses demonstrate the rise in Medicaid revenue for rural hospitals in Medicaid-expansion states may be protective against the rural hospital closures occurring in non-Medicaid expansion states. To improve rural care access, legislators in these states should expand Medicaid and raise the rates doctors are paid for seeing Medicaid patients.
Our findings have several implications for rural health outcomes and care delivery. First, the conventional view of ED visitation as only necessary for acute illness is far from reality in rural communities. This is a reflection of trends nationwide, where access to timely outpatient care is difficult and relies increasingly on EDs. Second, increased use of EDs by rural patients may complicate efforts to bolster chronic disease management and result in care fragmentation as ED care is usually not coordinated with primary care.
Policymakers should consider innovative payment and delivery models that integrate EDs into local health care delivery systems. This may improve patient access and coordination of care and reduce the cost. Examples of innovation in rural health care include co-location and mixed staffing models for rural EDs and global budgets for rural hospitals. Rural health faces many barriers, but we already see rural-centric innovation born from challenges to improve rural health.