In Summer 2019, our research team completed a scoping review of published articles and practitioner-focused grey literature to learn more about the intersections between immigration and health in the United States. Our research questions were: 1) What does the literature tell us about immigration and health equity in the US? and 2) What does the literature tell us about the role of immigration status as a social determinant of health? Mental health and wellbeing among immigrant communities emerged as key themes.
While we conducted the majority of this review before Covid-19 was first reported in the US, the ongoing pandemic has emphasized systemic and interrelated racial, ethnic, and economic inequalities in the US health care system and society more broadly. Our review identified several themes related to promoting health and wellbeing among immigrants and their communities, together with barriers to accessing services that should inform public health responses to Covid-19.
Therefore, it is imperative for established residents and new Americans to recognize that anti-immigrant stigma exacerbates the racial/ethnic health disparities in society at the local, regional, state, and national level.
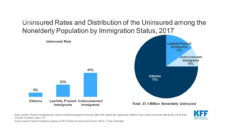
Immigration can be considered a social determinant of health for a variety of reasons. From a macro level, it is the structural racism and discrimination that result in well-documented health inequities. On a micro level, it is how a person’s immigration status influences their ability and eligibility to obtain health benefits and services. At the mezzo level, it is how these two ends of the spectrum come together as we examine the relationship between one’s own immigration status, mixed-status households, and ethnic enclaves that shape and reshape the living and working conditions for all community members. Factors like country of origin, destination country, race/ethnicity, age, socioeconomic status, and immigration status influence health outcomes both before and after migration and also impact the re-settlement process. Therefore, it is imperative for established residents and new Americans to recognize that anti-immigrant stigma exacerbates the racial/ethnic health disparities in society at the local, regional, state, and national level.
Our review findings fall into four themes related to mental health and wellbeing in immigrant communities:
- Disparities in mental health service use between immigrants and nonimmigrants;
- Impact of immigration laws on mental health and wellbeing for both immigrants and their family members across immigration and citizenship classifications;
- Unique considerations for adolescents and young adults; and
- Strengths-based approaches to addressing mental health needs.
We additionally found that immigration-related laws and policies change over time, which influences the mental health and wellbeing of both immigrants and nonimmigrants, especially members of racial and/or ethnic minority groups. For example, Latinx citizens and noncitizens living in a state with a high number of punitive immigration-related laws were less likely to report optimal health. However, studies that explored the connection between mental health and Deferred Action for Childhood Arrivals (DACA) suggested that DACA positively affected the mental health and wellbeing of young undocumented immigrants. However, after DACA, studies among undocumented Asian and Pacific Island youth and undocumented Latinx youth found that these groups still reported continued concerns about the deportation of family members who were not DACA-eligible.
Evidence from the studies we reviewed is relevant to policies and interventions related to Covid-19. First, identifying immigration status as a social determinant of health emphasizes the challenges many immigrants and their families face in accessing health services. Such challenges span immigration and citizenship classifications. Covid-19 response efforts must recognize the complex factors that affect health outcomes of different immigrant communities and be responsive to the heterogeneity of immigrant communities, including the diversity of their experiences. The US needs immigration integration efforts that intentionally encourage cooperation between newly arrived immigrants and longer-term residents. For example, Welcoming America’s initiatives, which focus on the connection between immigrant inclusion and health equity, can provide models for integration efforts. Public health practitioners, medical providers, and policymakers must work in partnership with communities to better understand immigrant communities’ health concerns. They must also recognize and build on the strengths and resources already present in those communities to support positive health outcomes.
Photo via Getty Images