Racial and ethnic disparities in health care are pervasive and persistent, including the care of children undergoing surgery. For example, among children with appendicitis, studies document that African-American children have a significantly higher risk than White children of delayed diagnosis, complications, and perforation. Distressingly, there is evidence that African-American children with minimal health problems undergoing inpatient surgery have three times greater chance of death within 30 days of surgery than White children.
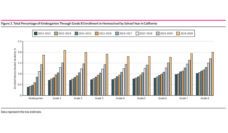
These studies prompted us to investigate disparities in access to surgery for minority children. We analyzed data from the National Health Interview Survey, a nationally representative database. We found that African-American, Asian, and Latino children were roughly half as likely as White children to have had surgery in the prior 12 months. For children who had surgery, we examined the type of surgery by race and ethnicity. We found differences in the types of surgery obtained, notably that Latino children were more likely to require urgent or emergent surgery.
Differences in receipt of surgery persisted even after we adjusted for common demographic factors such as insurance status, language, and poverty. Alternative factors likely contribute to the differences we found. Unfortunately, our study cannot determine the exact causes of decreased surgery among minority children, but possible explanations deserve discussion.
Our data indicate that minority children in the United States are less likely to report receiving surgical care.
How a family to interacts with the medical system and how the medical system treats families from different racial and ethnic groups likely impact the ultimate receipt of surgical care. Families of minority race and ethnicity may be impacted disproportionately by medical system distrust, communication difficulties with providers, poor health literacy, inability to take time off work, or transportation issues. For adults, these factors have been associated with worsened care in several areas including staged surgical care for lung cancer. Minority children are likely impacted in a similar fashion and perturbations of family structure, income, or insurance may disproportionately impact the care of minority children.
Finally, implicit bias within the health care system may affect minorities. Disparities in referral for pediatric subspecialty care and care coordination have been documented. Surgeries that require complex coordination require more interactions with health care systems and may introduce great risk of bias. This concern is evidenced by known disparities in access to pediatric kidney transplantation. Minority children may also be more likely to be seen by low volume health care providers or have decreased availability of pediatric surgical subspecialty care. Existence of these factors within pediatric surgical health care systems may affect diagnosis, referral, and treatment recommendations, as well as the type of surgical providers (low-volume vs high-volume) who ultimately operate on minority children.
Our data indicate that minority children in the United States are less likely to report receiving surgical care. These data raise the concern that minority children are less likely to receive indicated surgery at the most opportune time. Additionally, if surgery is omitted or delayed, minority children may have worsening disease that then requires more emergent care which carries more risk.
We hope that this work helps to reduce disparities in surgical access for minority children by raising awareness among clinicians. Increased monitoring will improve the likelihood that disparities will be identified expeditiously, stimulating rapid-cycle quality improvement and prompting further research. Every child in America deserves access to the right surgical care at the right time, regardless of skin color.
Photo via Getty Images