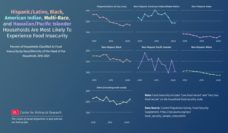
In 2021, 10.2% of U.S. households reported experiencing food insecurity. A year later, insecurity was at 12.8%, the first increase in years. This uptick represents 17 million households who struggled to put food on the table, didn’t have enough to eat, and weren’t sure when they would get their next meal.
A study by Sungchul Park and colleagues suggests that the challenges associated with food insecurity extend well beyond the feelings of hunger. The researchers analyzed data from more than 10,000 adults who participated in the Medicare Expenditure Panel Survey. They investigated how food insecurity, as reported by respondents in 2016, correlated with health insurance coverage, health care access and use, and financial hardship a year later.
In 2016, roughly 10% of respondents reported that they had experienced food insecurity. The following year, this group was more likely to be uninsured, to have lower access to care, and to experience greater financial hardship than persons who were food-secure. At the same time, food insecurity was also associated with higher health care use.
Recognizing the profound impact food insecurity has on overall well-being and health, numerous organizations across the U.S. have created programs to tackle access to food head-on. Kelsey A. Egan and colleagues evaluated one such initiative, the Preventive Food Pantry at Boston Medical Center (BMC).
Acting as the largest safety net hospital in the New England area, BMC serves a predominately low-income patient population, many of whom do not have easy access to perishable foods like fresh produce. So the Preventive Food Pantry connects patients who need these items to promote better health.
With the recent rise in food insecurity in the U.S., it is vital to explore and create innovative solutions that address the nutritional needs of diverse communities.
BMC’s pediatric primary care clinic routinely screens patients for food insecurity. If a patient reports struggling with food needs, their clinician can refer them to the on-site food pantry. The pantry is open on weekdays and is located in the same building as the pediatric clinic. Referrals allow patients to pick up three days’ worth of food every two weeks.
The authors found that not all of the patients who reported experiencing food insecurity received a referral to the food pantry. In a sample of 14,280 patients, 3,964 were food insecure. But only 1,517 received food pantry referrals, identifying a potential weakness in the referral process.
At the same time, not all referred patients accepted the referral. Only 28.9% of those who received referrals actually used the food pantry. The research team’s analysis indicates that some patients were more likely than others to use the food pantry, including those who received their referral during pantry open hours and those who lived closer to BMC. This speaks to practical concerns; patients may need to find transportation or other help to carry groceries home. But the authors note that there may have been other considerations (i.e., cultural factors or negative perceptions of food pantries) that impacted patients’ willingness to accept the resource.
Given the low use of food pantries nationally, some communities are considering other options to address food insecurity. For example, in Chicago, Mayor Brandon Johnson is considering opening a municipally-owned grocery store to promote food equity in hard-hit areas of the city. In Philadelphia, two residents are creating The Community Grocer, a nonprofit grocery store that offers low-income residents an affordable, high quality, hot meal instead of pantries’ usual supplies of highly processed foods.
With the recent rise in food insecurity in the U.S., it is vital to explore and create innovative solutions that address the nutritional needs of diverse communities.
Photo via Getty Images