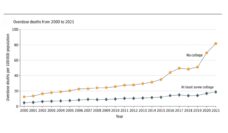
Fenway Park holds 37,755 seats. A sold-out game, filled with many thousands of cheering fans, would make up less than half of the 80,000 people lost to opioid overdose in 2021. Drug overdose has cut 1 million lives short over the past 25 years, with half of these deaths from opioids.
People using opioids face an increasingly dangerous supply, with an increased presence of fentanyl spurring more overdoses. Opioid injection leads to additional medical complications, like Hepatitis C, HIV, and bacterial infections. Despite increasing emergency room visits for drug use-related infections, an estimated 9 out of 10 individuals with an opioid use disorder are not receiving any treatment. Long wait times, administrative burdens (like treatment contracts or insurance authorizations), inadequate support, and past stigma in health care settings all stand between patients and their path to care.
Jessica Taylor and her colleagues recently explored the use of bridge clinics, which have emerged as innovative treatment models of care that cut through challenges that opioid users have faced in other care settings. These new medical programs lower barriers to treatment entry and promise a greater focus on each person’s needs and their medications for opioid use disorder (MOUD; e.g. buprenorphine or methadone) treatment. The goal of these clinics is to offer immediate and on-demand access to medications, to reduce overdose, and to keep people engaged in long-term treatment.
Bridge clinics are often based in outpatient hospital settings. They provide clinical care, harm reduction services, or behavioral health support to individuals. Within the same institution, providers can form an interdisciplinary team: infectious disease experts can help patients with injection-related infections; addiction medicine physicians can assist with treatment plans; and nurse practitioners can manage care.
If the evidence of success for bridge clinics continues, this model may soon expand and perhaps cut into the number of preventable deaths of the opioid crisis.
Patients at bridge clinics have greater access to hospital departments, which can prevent long wait times and allow for scheduled drug administration (like methadone) or more expensive treatments (like extended-release injectable buprenorphine) to be started right away. Some of these clinics incorporate additional care (e.g. wound treatment, screening and testing for viral and bacterial infections, including HIV or sexually transmitted diseases), medications to treat and prevent infections (e.g., antibiotics or PrEP), and vaccines. Bridge clinics also value harm reduction services, such as overdose education, naloxone distribution, and safe injection training and materials
Emergency room‐based bridge models provide immediate care after hours. In these models, patients are given an MOUD prescription and take-home harm reduction kit with instructions to follow up in the clinic. These actions have helped sustain care and reduce repeated emergency department use.
Virtual bridge clinics, a necessity during the pandemic, allowed MOUD treatments without the need for in-person visits. Telemedicine-based treatment initiation and access to providers have remained useful for those with limited travel options. Virtual clinics based out of New York and Rhode Island worked with unhoused and formerly-incarcerated individuals, groups that are historically difficult to reach.
People with mental illness and mood disorders, people with high rates of sexually transmitted diseases, people who are unhoused, and people who use multiple substances are all commonly seen at bridge clinics. Bridge clinic staff often include peer recovery coaches, who offer a more personal support to patients.
Outcomes from patients in bridge clinics demonstrate clinical benefits. MOUDs aid in decreasing opioid use and risk behaviors associated with using needles (like testing positive for HIV or Hepatitis C). Importantly, patients in bridge clinics show improved follow up—since many persons with substance use disorder leave care prematurely—with a Treatment Improvement Protocol, with 80% of patients in these models following up within 30 days. Follow up was also present in antibiotic course completion for those diagnosed with an infection at their initial visit.
For now, most bridge clinics are found in large cities across states that have expanded Medicaid coverage and within institutions that support individuals with substance use disorder. If the evidence of success for bridge clinics continues, this model may soon expand and perhaps cut into the number of preventable deaths of the opioid crisis.
Photo via Getty Images