Public Health Post: What does it mean to you to be mentally well?
Dévora Kestel: The definition of mental health that we use at the WHO is having a productive life, coping with challenges and stressors, and being a contributing member of the community. It is not only the absence of a disease.
We have been saying for a while that there is a continuum between being mentally well and having a mental disease. Depression is a good example. There’s a lot of room between being sad and being clinically depressed and active suicidality. Being sad is, of course, not a disease- you can be mentally well and be sad. A binary between mental wellness and mental illness is too simplistic.
How does the WHO adapt to the many different understandings of mental illness and wellness globally?
In a non-Covid year, ministers of health from each of the 194 member countries would come to Geneva, and we would present about the importance of mental health services and policies. When they leave, we have an agreed-upon action plan that those countries are working on at the country level with both clinical and public health components. We try to incorporate people with lived experience as much as possible, so that the discussion is adaptive to what’s happening on the ground.
Can you speak to the role social determinants have to play in shaping our mental health?
We understand that social determinants, and poverty in particular, have a role to play in mental diseases and disorders. have a role. Alleviating poverty and creating better contexts can prevent mental illness. But it does beg the question- is alleviating poverty mental health professionals’ responsibility?
What are some of the structural barriers to mental health access globally?
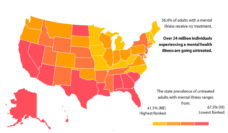
Only 2% of the health budget globally goes to mental health. So mental health services are very limited compared to other health services.
From that two percent, the vast majority of the funds go to old-fashioned mental institutions and psychiatric hospitals, places where violations of human rights take place on a regular basis. It’s not only a question of the quantity of mental health facilities, but also the quality.
Additionally, very few professionals specialize in mental health. Traditionally, mental health has been treated as exclusive knowledge of psychiatrists and psychologists and occasionally a subset of social workers and nurses. But that’s it. Nobody else is supposed to deal with mental health. This is slowly changing. Ideally, every health professional and social services professional would have some basic mental health knowledge, and people would be more likely to access services as they needed them.
Photo courtesy of Dévora Kestel
If you are having thoughts of suicide, call the National Suicide Prevention Lifeline at 1-800-273-8255 or visit suicidepreventionlifeline.org.