How many minutes now? Long enough for your eyes to strain. You’ve been staring at those two blue lines knowing what they mean but your mind has been in another place. You know what you have to do, but experience tells you cold turkey is living hell. Stomach twisted. Dry heaving. Diarrhea — the violent kind. You’ve heard that methadone or buprenorphine can help you manage the withdrawal, but you’re terrified about how the doctor will react to a pregnant woman addicted to opioids. Where do you go?
Buprenorphine and methadone are so instrumental to saving lives and improving health for persons with opioid use disorder that the US Surgeon General in 2016 declared increased access a top public health priority. Increased access to buprenorphine and methadone especially benefits pregnant women and their unborn infants. Providing these medication to manage opioid withdrawal symptoms enables women to decrease the pain of addiction enough to focus on other aspects of their health and pregnancy, leading to the improved health of the child and lower risk of birth defects, preterm delivery, and stillbirth. The ability to receive these medication treatments depends on where pregnant women seek care. Clinicians with a special federal waiver can prescribe buprenorphine, but methadone is only available in federally regulated opioid treatment programs where complex medical care is not routine.
Steven Patrick and his team wanted to know if pregnancy is a barrier to opioid use disorder treatment and if the type of treatment or payment method matters. Nine “secret shoppers” made over 10,800 calls to buprenorphine and methadone prescribers across 10 states. Callers claimed to be either four-months pregnant or not pregnant; similarly, they offered to pay for care using Medicaid or private insurance, which typically reimburses more generously.
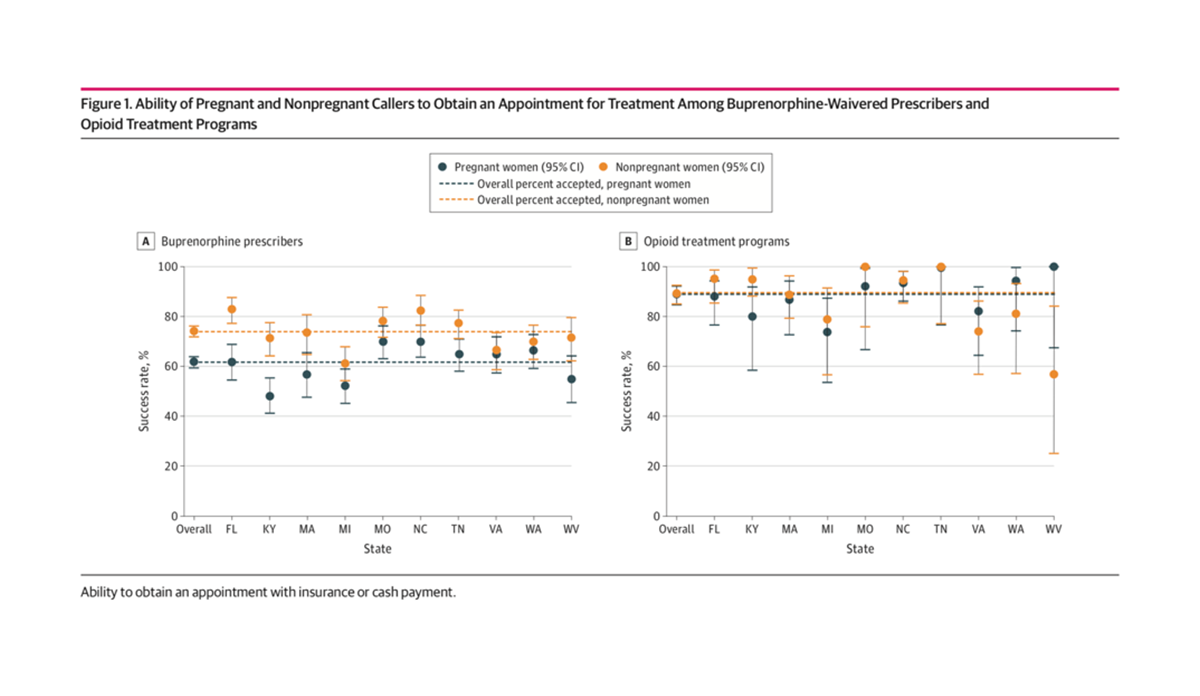
The left graph above shows that pregnant callers were 17% less likely than non-pregnant callers to successfully secure an appointment with a buprenorphine prescriber. The graph on the right indicates that pregnancy status was not significantly associated with securing an appointment with a methadone prescriber. Payment type only mattered for non-pregnant callers, who were less likely to get an appointment with a buprenorphine prescriber if they said they were insured by Medicaid.
Patrick and his team note that few buprenorphine prescribers specialize in women’s health. They speculate that this lack of experience and familiarity with women’s health might reduce the willingness of clinicians to provide addiction-related care to pregnant women.
Databyte via Patrick SW, Richards MR, Dupont WD, et al. Association of Pregnancy and Insurance Status With Treatment Access for Opioid Use Disorder. JAMA Netw Open. 2020;3(8):e2013456.