By the end of 2020, 18.5% of global COVID-19 deaths came from the U.S. At this time, we ranked higher in COVID-19 deaths than France, Germany, Mexico, and Brazil. Part of the reason for our high COVID-19 mortality was due to the lack of a uniform, national public health response. States, counties, and cities were required to create their own steps for monitoring COVID-19 infections, administering COVID-19 tests, and handling COVID-19 surges in hospitals. This, inevitably, led to gaps in the overall public health response across America.
Throughout the pandemic, research showed worse COVID-19 health outcomes among racial and ethnic minorities and those with lower incomes; however, there was no investigation into how differing state and local public health systems could have influenced COVID-19 deaths. Given the variation in COVID-19 processes across states and localities, we decided it would be worthwhile to study how existing capacity, resources, and funding might impact a locality’s ability to handle COVID-19.
Previous research around U.S. local health systems shows that the communities they serve have fewer preventable deaths when they offer a wider range of public health activities (e.g., investigation of disease outbreaks, surveying the community for health needs, etc.) and have more organizations (e.g., hospitals, K-12 schools, health insurers, etc.) involved in those public health activities. We define these two areas as the local health system “capability” score.
Many local health systems argue that their capability score should not be compared to other systems, since each is responding to the unique needs of their community. Some communities might focus more resources towards advertising about opioid addiction treatment centers rather than investigating a measles outbreak at a local school. Under our definition, the local health system that is performing both activities would have a higher capability score, even when it might be more appropriate to only deliver one activity given funding and staffing limitations.
It seems that we have not learned our lesson even after a global pandemic has so far killed over 1 million Americans.
However, the pandemic provided a rare opportunity to directly compare the local health system capability to a common outcome: COVID-19 deaths. During 2020, most local public health systems across the country were delivering activities that would stop the spread of COVID-19 and reduce the overall burden among those infected. This made each local public health system more comparable under our definition.
Through our analysis, we found that, at the end of 2020, there were 18.1 more COVID-19 deaths per 100,000 residents among counties with the lowest public health system capability score versus those with the highest capability score.
These findings support previous calls to increase funding for local public health systems to assure that local health systems have the resources necessary to support delivering additional public health activities and partnering with more organizations. Especially before another public health emergency like COVID-19 occurs.
It seems that we have not learned our lesson even after a global pandemic has so far killed over 1 million Americans. A recent report showed a 3.5% decrease in federal health care expenditures during 2021. This decrease happened while many counties and cities were still experiencing surges in COVID-19 deaths due to the Delta and Omicron variants. Funding and resources should be increased back to pandemic levels, if not higher for those public health systems with lower capabilities. The increased funding will prepare these local health systems to fight against future infectious disease outbreaks and other public health emergencies.
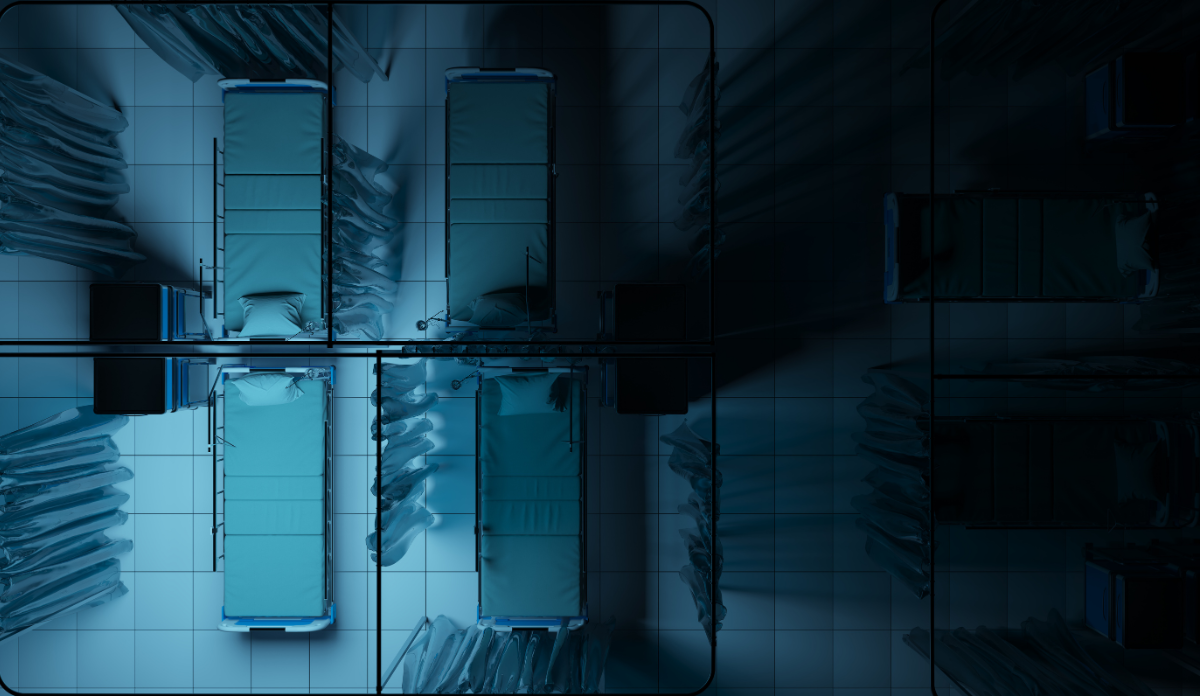
Photo via Getty Images