The Center for Medicare & Medicaid Services (CMS) recently released guidelines for states interested in implementing Medicaid work requirements. The guidelines advocate for improving “work and community engagement” by making it a requirement for Medicaid eligibility. In other words, people would need to be deemed “engaged” in order to be eligible for Medicaid in interested states. The new Medicaid work requirement proposals further an ongoing dialogue about who is deemed deserving of help in the U.S.
Work requirements are not a new idea. Ronald Reagan famously coined the term “welfare queen” back in the 1970s referring to a single case of extreme welfare fraud in Chicago to urge welfare reform. Subsequent reform in 1996, during Bill Clinton’s presidency, replaced relatively broad eligibility for food stamp benefits with three months of benefits through the Supplemental Nutrition Eligibility Program (SNAP). SNAP tied eligibility for food aid to participation in work or work training in 36 month chunks of time. In other words, SNAP recipients who did not work or participate in a training program were cut off after three months.
The idea underlying SNAP and similar policies comes down to the belief that beneficiaries are taking advantage of these public programs—living off of government benefits without lifting a finger. Research from the University of California Berkeley Labor Center suggests otherwise. The center estimates 73% of enrollees in American public benefit programs are from working families. Working families are defined as having at least one family member who works 27 or more weeks per year and 10 or more hours a week. Most of these workers are in low-wage occupations such as fast food workers, child care providers, and home care workers.
Medicaid Work Requirements
Medicaid eligibility as outlined by the CMS would require “work and community engagement among non-elderly, non-pregnant adult Medicaid beneficiaries who are eligible for Medicaid on a basis other than disability.” The working theory is that work and community engagement will improve overall health. They list other social determinants of health, such as education, as examples of factors that improve health. Higher levels of education clearly correlate with better health outcomes. But health problems can disrupt children from attending school, thus affecting academic performance. The same can be said of employment. Sure, “higher earnings are positively correlated with longer life span.” But causality can move in the other direction as health problems can hinder ability to work and lead to unemployment.
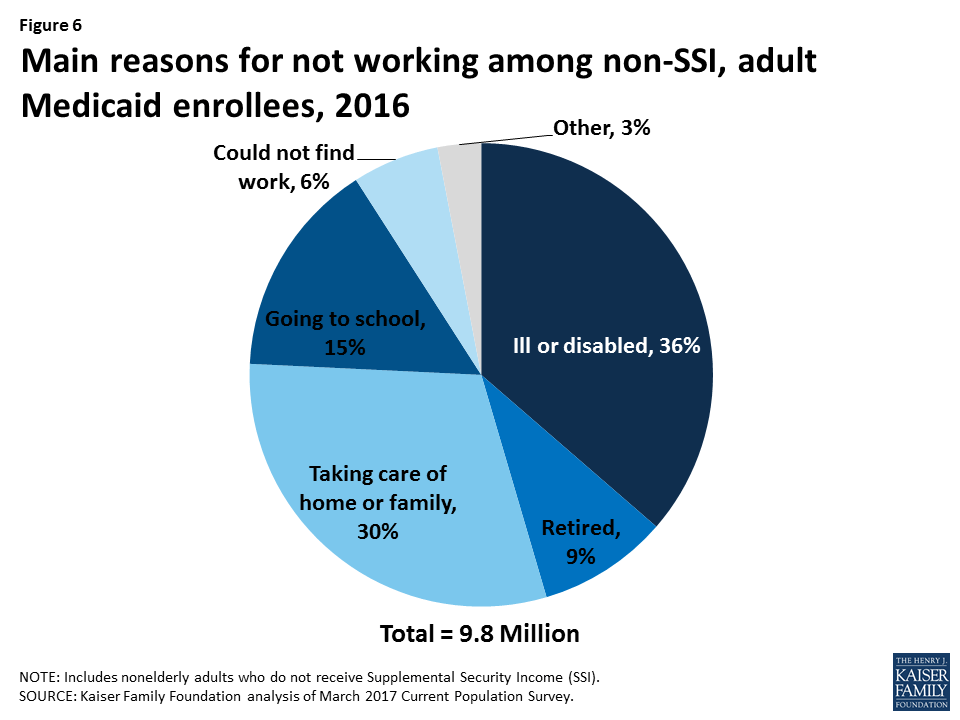
At the heart of this policy is the speculation that many Medicaid beneficiaries can work but choose to stay unemployed. Data from the Kaiser Family Foundation indicates the opposite. Most Medicaid enrollees have good reasons why they are not working. As depicted in the figure, most are ill or disabled or taking care of home or family. Only 6% could not find work. What this means is that these extra hurdles imposed to gain eligibility could be a barrier to many who should be eligible and need the insurance. The CMS guidance does not adequately address how states would check for eligibility and support citizens attempting to meet eligibility.
Currently ten states have submitted work requirements. Kentucky’s Section 1115 waiver to implement Medicaid work requirements, approved on January 12, was the first of its kind. States like Wisconsin and Kentucky have proposed changes such as drug-testing and requirements for beneficiaries to pay more out-of-pocket. Kentucky also proposed a controversial health or financial literacy course to re-enroll in Medicaid should you fail to meet work requirements. Details are still hazy for the courses and their mandatory quizzes. But, as Austin Frakt points out, many Americans, not just Medicaid enrollees, would struggle with a health or financial literacy test.
These families will make too much money to be eligible for Medicaid and not enough to qualify for ACA marketplace assistance which starts at 100% FPL ($16,400 annually).
Medicaid enrollees in states that have yet to expand Medicaid will face a unique challenge. Medicaid expansion raised the federal poverty level (FPL) for eligibility in participating states to 138%. Eligibility in non-expansion states is much more difficult with typically lower qualifying federal poverty level. For example, Mississippi is a non-expansion state that has submitted a work requirement waiver for its Medicaid population. A parent in a family of two (or a single parent with a child) must have an annual income under 27% FPL to qualify for Medicaid, which is about $4,385. The $7,540 salary for working at least 20 hours per week at minimum wage ($7.25 per hour) would disqualify families from assistance. These families will make too much money to be eligible for Medicaid and not enough to qualify for ACA marketplace assistance which starts at 100% FPL ($16,400 annually).
By the Bootstraps
The CMS guidance on Medicaid work requirements is another example that help is not given to those who need it the most. Medicaid work requirements are sold as welfare reform under the belief that the undeserving poor are doing nothing to improve their circumstances. Thus, help should only be offered with many strings attached. Elizabeth Bruenig, a journalist with the Washington Post, observes that help in the form of tax breaks and subsidies is readily given to the wealthy without a discussion of whether they are lazy or deserving. Yes, the American government spent $200 billion on Medicaid in 2012. But, the government also lost out on $120 billion by subsidizing employer-sponsored health insurance.
The phrase “by the bootstraps” reflects this feeling that the poor must be lazy if they cannot pull themselves out of poverty. I am not downplaying the accomplishments of people who have started with nothing and made a comfortable living for themselves. However, not everyone is able to pull themselves up by the bootstraps due to a variety of circumstances. Often, systematic and structural obstacles stymie their efforts to achieve a comfortable life. Under work requirements, a beneficiary could have Medicaid revoked due to either failure to comply with community engagement or absence of paperwork. We are asking the impossible of the poor in the U.S.: become successful while being locked out of essential services. So, who is deserving of help? According to the Medicaid work requirements guidelines, only the poor who are able to consistently hop over tall hurdles.
Feature image: Ben Lelis, The Mop, used under CC BY-NC-ND 2.0