
2021 Year in Review
Executive Editor Michael Stein reviews the most talked about posts of 2021, announces the 2022 PHP fellows, and says goodbye to the 2021 fellows.
...more
Executive Editor Michael Stein reviews the most talked about posts of 2021, announces the 2022 PHP fellows, and says goodbye to the 2021 fellows.
...more
The Period Project provides free pads and tampons, information about period poverty, and advocates for equitable access to these very necessary items.
...more
Paul Shafer announces our 2022 student essay contest and talks about what happened in health politics since his winning essay five years ago.
...more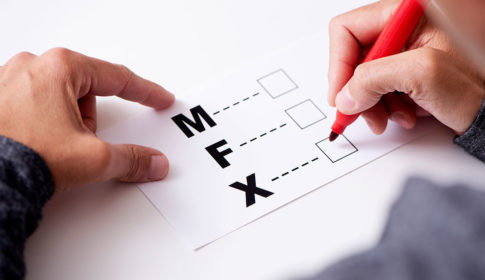
Every state should offer an “X” designation and make the process of changing one’s gender marker easy and accessible.
...more
When success for athletes is defined as winning and playing time, where does mental health come in?
...more
The authors highlight recently passed Massachusetts environmental justice legislation and its implications.
...more
Public Health Post honors a great writer — founder David Jones — by asking those he taught to share their memories, in writing, of course.
...more
Public Health Post honors the life of founding Editor-in-Chief David Jones.
...more
A first-generation immigrant challenges Latinx to talk about mental health and shares her own story.
...more
We need to strengthen and build robust health data utilities that can link and connect public health and clinical data systems.
...more