Misinformation leads to ill-advised public health approaches to treating obesity. At least three quarters of media reports emphasize “individual responsibility” even though most scientific papers argue that obesity is the culmination of many factors often outside one’s control. The will-power myth and others lead to common misunderstandings of the role of weight in health.
One such myth is that body mass index (BMI) indicates healthy or unhealthy weight. Though it incorporates height and weight, BMI is an inaccurate predictor of health. This is especially true for people of color, because BMI thresholds were based on Western European body types. BMI also does not account for weight distribution, nor can it differentiate between adipose tissue and muscle.
BMI is the sole mechanism used to determine obesity. Some argue that using a single BMI-based definition of obesity allows for uniform data tracking. This is true, given that BMI is an appropriate standard to measure how the average size of a population changes over time. However, it’s widely overused in individual health. While it can be one of many data points informing a patient’s care, given its flaws, BMI should not be the sole factor to determine whether a person’s weight is a health concern.
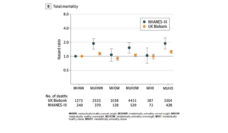
What’s more, the actual causation between illness and obesity is not clear. While data can point to an association between illness and obesity, causation is yet to be proven. The three diseases most commonly associated with obesity are heart disease, hypertension, and diabetes, yet there is little evidence to demonstrate how a BMI categorized as overweight or obese causes these diseases.
This idea is best illustrated by studies that control for income when analyzing health. For example, when controlling for income, those who are overweight and moderately obese actually have a higher life expectancy than those with a normal or low weight, suggesting that environment rather than obesity is a causal factor. This may also be due to something called the “obesity paradox,” where overweight and moderately obese people are better protected from illness. For instance, an obese person is more likely to survive a heart attack than an individual in the normal weight range. An obese elderly individual is also better protected from falls and osteoporosis than someone who is not obese.
The relationship between weight gain and health should be subject to more investigation.
This information should not diminish the challenges of living with obesity. Instead, it is meant to highlight that the relationship between level of weight gain and poor health should be subject to more investigation.
Although losing weight is often the gold standard for getting healthy, there are no long-term studies demonstrating that weight loss improves health. Because long-term weight loss seems nearly impossible for most people, it is a poor approach to sustained health improvement.
Furthermore, the stress associated with dieting often leads to higher blood pressure. This suggests that a doctor would be better off prescribing healthy lifestyle changes to those with the goal of improving their general health, rather than encouraging them to go on a diet or prioritize weight loss.
Given the misconceptions surrounding BMI and obesity, it is important to consider other means of measuring and promoting health. For example, Health at Every Size (HAES) offers an alternative to traditional obesity treatments by encouraging weight neutrality and promoting individualized healthy choices. HAES participants experienced sustained increases in physical activity, improved overall mental health, body confidence, and improved blood pressure. The evidence to support this approach is limited due to most study participants being white women. However, this research provides promising insight into what successful health promotion could look like, in contrast to traditional obesity treatments which remain largely unsuccessful.
Photo via Getty Images