In general, children are healthy. In fact, almost every major category of disease has an onset that occurs after young adulthood. The sole exception is mental illness. These conditions are relatively common in young people. In the 2010 Global Burden of Disease study, mental health disorders accounted for well over half of disability adjusted life-years in youth, ages 10-24, in high-income countries. That is, the greatest disease burden in youth from high-income countries is related to their mental health functioning.
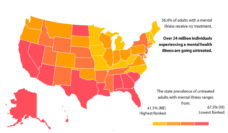
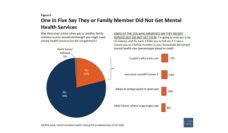
Unfortunately, most children with mental health problems (~60%) never receive any services at all, and their problems go undiagnosed and untreated. These children and their families are left to cope on their own. Among those who do access care, many only receive services in schools rather in a primary care or specialty mental health setting.
This dire dilemma raises a tantalizing opportunity. What would happen if all (or even most) children with mental health problems received the services they need? How would this treatment improve the lives of these children and their families? And, perhaps most important, how would such early intervention affect their risk for mental health problems later in life? This notion is called the ‘intervention as prevention’ hypothesis. Like many such thought experiments, it has never been tested.
My colleagues and I sought to fill this gap using the Great Smoky Mountains Study, which has been tracking a cohort of children for the past 25 years. This study has assessed both child mental health and mental health service use multiple times during childhood using “gold standard” structured interviews. This allowed us to compare children with mental health problems who received treatment to those with similar problems (and life circumstances) who did not receive treatment. The question was simple: Would childhood treatment prevent mental health problems in adulthood?
Like many simple questions, the devil is often in the details. Here, we had to consider the type of mental health problem (for example, depression or ADHD) as well as the severity of those problems. We also had to consider the type of services the child received, as well as how long they received the services. Did they receive ongoing individual psychotherapy from a psychologist for six months or a handful of medical checks from their primary care physician?
In the end, the results were the same, regardless of what type of mental health problem, the severity of the problem, the type of service received, or the length of service use. Those who received childhood treatment had similar levels of mental health problems in adulthood as those who received no such services. In a few cases, they were worse off.
These findings were disappointing. There is every reason to want early intervention to yield positive benefits that extend across the lifespan, particularly when we are talking about mental health problems that exact a heavy toll on individuals and their families. This is the long-extolled promise of early interventionists: a small investment for a large gain over a long period of time. Our results suggest that with mental health intervention – like so many other areas of life – there is simply no silver bullet.
Reducing the burden of mental illness across the lifespan is complex. It requires strategies to identify mental health problems early in the disease course. It requires prevention programs that target early risk factors, such as poverty and early adversities. It requires a mental health service system that provides treatment at each part of the lifespan and across key transitions. Finally, it requires a quiver of evidence-supported interventions. Such efforts have the potential to relieve distress and improve functioning. But, mental health, like physical health, is a lifelong challenge.
Photo via Getty Images