Taxi and for-hire vehicle (FHV) driving is a fast-growing occupation in the US, fueled in large part by the rapid adoption of ridesharing. New York City alone has 185,000 taxi, traditional FHV (limousine and black livery cab), and app-based drivers. Most are immigrant and underrepresented men who often work 10 to 12 hours per day, six days per week. They frequently experience sleep disturbance, high blood pressure, overweight/obesity, elevated particulate matter exposure, and poor access to health care. These factors increase drivers’ risk for chronic diseases such as diabetes, cancer, and cardiovascular disease.
Taxi, traditional FHV drivers, and those who drive for ridesharing services report that stress is a primary barrier to health and job satisfaction. Work-related stressors include racial discrimination, health concerns, passenger harassment, safety threats, bathroom inaccessibility, and excessive ticketing/traffic fines. Additionally, the driving industry has undergone tumultuous changes with the advent of ridesharing, which has put downward pressure on drivers’ income. Given the increased stress caused by these changes, and the many other stressors and health risks that drivers face, understanding and addressing their health is of critical importance.
Because taxi and FHV drivers lack time outside work to attend to their health, workplace screenings and interventions can improve health behaviors by increasing physical activity and primary care uptake. However, interventions to simultaneously address multiple health behaviors and decrease stress would be ideal. We designed a study to gain a better understanding of the relationship between perceived stress, demographic factors, and health behaviors in a sample of NYC taxi and FHV drivers.
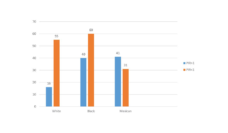
Two hundred fifty-two drivers participated in our cross-sectional survey. Most were men, mean age 45 years, who hailed from South Asia (mainly India, Pakistan, Bangladesh), Latin America, and Africa. Seventy-five percent spoke limited English (reported speaking English less than “very well.”) Most drove yellow medallion (55%) or green street-hail (45%) taxis, and the rest (3%) drove traditional FHVs. Over half (55%) of the drivers experienced moderate or high stress, as measured by the 10-item Perceived Stress Scale.
Drivers who reported speaking English very well had lower stress levels than drivers who spoke limited English. They were also more likely to engage in moderate and vigorous physical activity. Limited English proficiency has been associated with psychosocial distress among Asian and Latino immigrants. Immigrants with limited English may find it harder to communicate with others, create social networks with English speakers, and access information, undermining their lifetime socioeconomic opportunities.
Our study found that stress predicted sleep disturbances among drivers. More than half slept less than the recommended seven hours per night minimum, and 16% reported five hours or less. Long working hours likely contributed to drivers’ lack of sleep. Health risks of inadequate sleep include cancer, cardiovascular disease, and driving accidents.
Few participants met the Centers for Disease Control and Prevention recommendations for moderate to vigorous physical activity and daily fruit and vegetable consumption. This can exacerbate risk for cardiovascular disease, cancer, and diabetes. Studies have found evidence that stress is associated with poor diet and low physical activity.
Our findings compel multilingual interventions for taxi and FHV drivers to tackle stress and to improve driver sleep, diet, and physical activity behaviors. The optimal approach may be to offer a range of occupationally tailored interventions selected and packaged according to individual driver needs. For example, a stress-management intervention could include breathing exercises that can be done in the cab and case management to help ameliorate socioeconomic sources of stress, such as housing instability and food insecurity. This could be delivered alongside diet, physical activity, sleep, and healthcare access components, as needed.
Stressors on NYC taxi and FHV drivers have increased since we conducted our initial research from 2014 through 2016. Taxi medallion devaluation has left thousands of drivers with overwhelming debt, was linked with several 2019 driver suicides, and prompted a recent taxi driver hunger strike. The socioeconomic impacts of industry change, reduced earnings, and the COVID-19 pandemic have been devastating for drivers. The need for driver health interventions is urgent and potentially greater than ever.
Photo via Getty Images