Whether you are a scientist, chef, or just a person on a healthy weight journey, scales play some role in your life. We all trust scales to give us unbiased measurements of weight when we need to understand it more clearly.
Most often we associate the use of scales with changes in body weight. The World Health Organization classifies anyone with a body mass index (BMI) greater than 25 as overweight and anyone with a BMI greater than 30 as obese. According to the CDC, Black adults have the highest prevalence of obesity in the United States, after adjusting for age. Previous studies have found that BMI trajectory, anticipated weight patterns, are linked with social disadvantage. Educated white men have the lowest BMI increase and Black women have the highest.
Racism takes many forms. Interpersonal racism (i.e. using racial slurs, hate crimes, etc.) is most commonly understood because it is most visible. Yet structural racism, defined as institutional policies and actions that result in detrimental treatment for members of a particular racial group, is arguably more harmful and less visible to the untrained eye.
When race is used in research, it serves as a rough proxy for socioeconomic status, culture, and genes. Racial categories describe the social classification of people living in a race-conscious society, rather than an innate biological difference. But race is not a source of health vulnerability or risk. Racism is.
The consistent exposure to social and environmental stressors due to racism results in chronic inflammation and subsequent disease, including obesity.
Previous studies have focused on housing segregation, poverty, employment or incarceration—common products of racism—and their influence on obesity. But which of those factors can be measured to truly quantify the experience of racism?
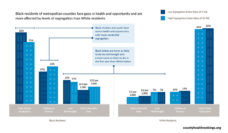
Dougherty and colleagues believe that structural racism is an underlying construct that prompts discriminatory practices. Structural racism is too complex to be accurately captured by any singular factor. So, they used a 5-domain scale to measure racism at the county level in the United States and evaluated its association with BMI.
The researchers selected housing, education, employment, health care, and criminal justice as the relevant domains, because they directly impact access to the resources needed for better health outcomes. Access to nutritious food safe, activity space, quality health care knowledge and money are all impacted by structural racism. Therefore, the investigators used data from the 2011 and 2012 Behavioral Risk Factor Surveillance System to assess each domain on the county level.
Overall, county structural racism was associated with lower BMI in white people and heightened BMI in Black people. Structural racism is negatively associated with BMI across counties throughout the nation, driven by the large proportion of white people in most counties.
The researchers also looked at the combined influence of race and gender on BMI. County structural racism was associated with larger increases in BMI among black women than black men. County structural racism was also associated with reduced BMI for white men although there was no change for white women. These findings support previous findings that indicate both that race and gender contribute to social disadvantage and increased BMI.
Investigators have grown more interested in the link between BMI and structural racism which is often seen in the differences that white and Black people have regarding access to healthy foods, differences in knowledge about healthy eating practices, opportunities for physical activity, and discriminatory housing policies that segregate Black people into lower-resourced areas.
Other researchers have focused on more proximal mechanisms of racism, such as weathering. The process of weathering is a metaphor for erosion of health caused by chronic stress. The consistent exposure to social and environmental stressors due to racism results in chronic inflammation and subsequent disease, including obesity.
It is racism, not race, that underlies differences in health outcomes. Regardless of how heavy the burden of inequity may feel, it can be measured. But sometimes you just have to tip the scale.
Photo via Getty Images