The “gender paradox in suicide” is a persistent trend in which women attempt suicide more than men, while men complete suicide at higher rates. This trend is constant on a global scale—the average rate of completed suicide is 15.0 per 100,000 deaths for males worldwide, and 8.0 per 100,000 deaths for females.
The paradox has been widely acknowledged since researchers Dr. Silvia Sara Canetto and Dr. Isaac Sakinofsky published an article in Suicide and Life-Threatening Behavior in 1998. That same year, the U.S. Centers for Disease Control and Prevention released a National Vital Statistics Report which showed that “the greatest sex differential in age-adjusted death rates was for suicide, with a mortality sex ratio of 4.3 male deaths to 1 female death.”
Since then, suicide rates have continued to rise in the U.S. for males and females for all age groups under 75.
According to the most recent NVSR death report released June 2016, the gender discrepancy has fallen slightly. As of 2014, men died by suicide 3.6 times as often as women. It is the 7th leading cause of death for males, and is not listed as a top 10 cause of death for females. The American Association for Suicide Prevention also points out that white males accounted for 7 of 10 suicides in 2015.
It has been nearly 20 years since the Gender Paradox was first acknowledged. Suicide rates are getting worse, and men continue to bear the brunt of the tragedy.
In Canetto and Sakinofsky’s pivotal 1998 research, they consider that “the belief that killing oneself is masculine may serve as a facilitating factor”. They explore four possible explanations for the phenomenon:
- Lethality – methods are gender specific and males are more likely to employ more lethal means
- recall bias – “women are ‘better reporters of health history’”
- differential rates of depression and alcohol abuse – women are treated more for depression and men are more likely to abuse alcohol)
- socialization – society associates certain traits as being “male” or “female,” which fuels expectations of masculinity and femininity
Ultimately, they reason that cultural expectations are the most influential and testable explanation.
“Cultural expectations about gender and suicidal behavior function as scripts,” they explain. “Individuals refer to these scripts as a model for their suicidal behavior, and to make sense of others’ suicidal behavior.”
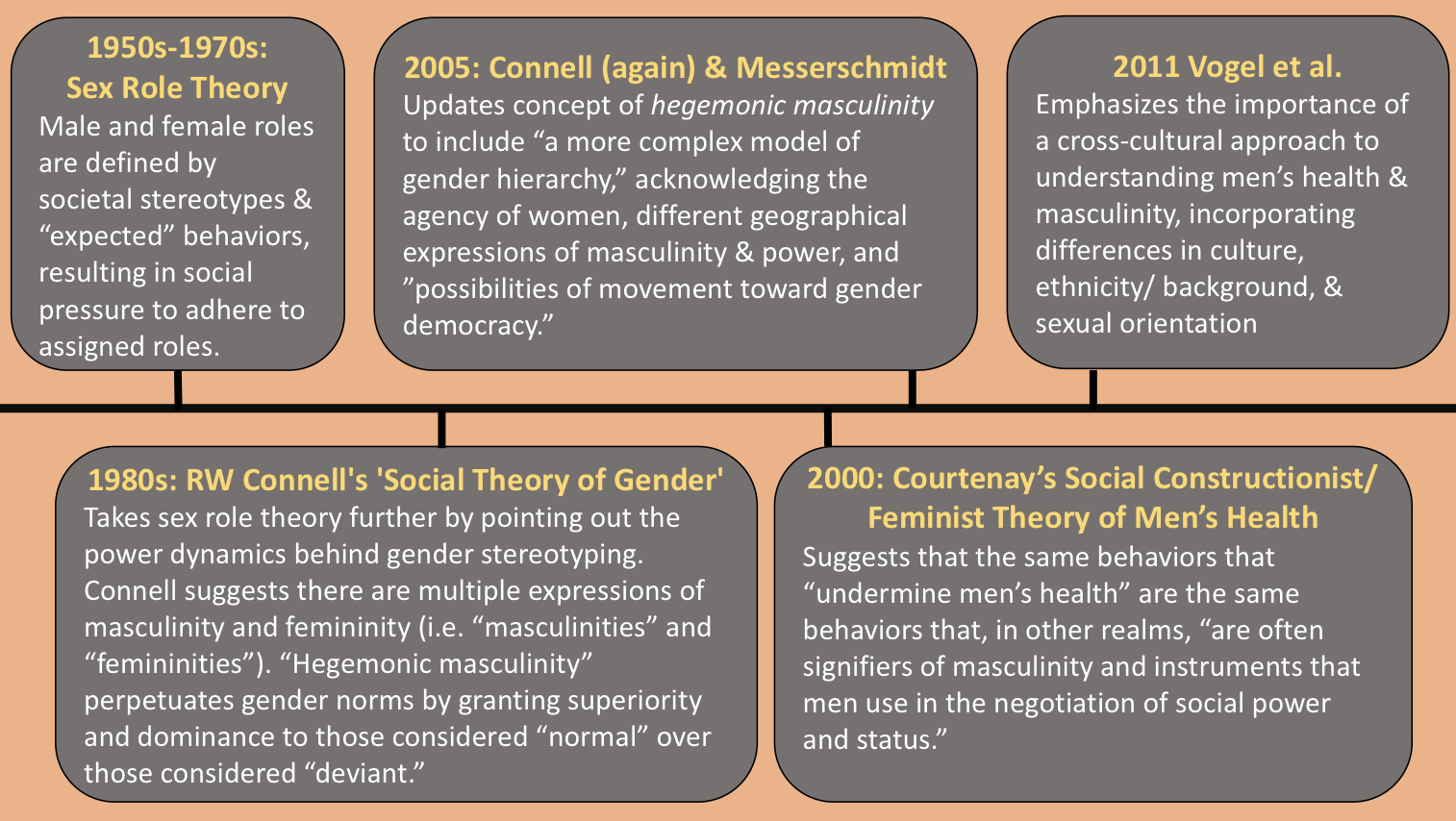
A brief theoretical timeline of masculinity and men’s health
Applying theory to practice in suicide and mental health: Why it matters
Theory and the observation of “masculinity”—in all the many ways it can be defined or played out—can offer insights into how to care for the mental health, and the general health, of men. Because there are many means of expression for masculinity and femininity, there must also exist a broad spectrum of interventions and approaches. The first step seems to be recognizing and, even more importantly, normalizing the idea that ‘maleness’ is a risk factor for untreated mental illness and suicidality.
Since the mid-1990s and early 2000s, many studies have emerged that support the relationship between masculinit(ies) and the tendency not to seek help in instances of mental illness, or even physical help. Most of them conclude that acknowledging this relationship can inform “future interventions.”
Very few of them, however, offer possible solutions. The few that do have suggested men’s groups; media campaigns that portray depression and mental illness as challenges that are not specific to a “better” or “worse” expression of masculinity; encouraging men to seek out various social networks so as to be more likely to find acceptance in his help-seeking behaviors; increasing the tendency for potential helpers to take suicidal threats seriously; and focusing on adolescent boys and how society socializes them.
Where do we stand today?
Since the beginning of 2017, researchers have produced several articles that continue to explore gender differences in suicide. They address barriers to seeking help, such as the social stigma against suicide, wherein society tends associate suicidality with weakness or selfishness; and the fact that men with the most severe symptoms of depression also hold the most “negative attitudes towards help seeking.” Another tested hypotheses related to self-stigma as a barrier to help-seeking in an experimental study. Its results supported that internalized gender stereotypes do tend to keep men from seeking help, and urged health interventions and campaigns to take these tendencies into account moving forward.
Only one study, which was also coauthored by David L. Vogel, provides a much-needed tangible suggestion for the development of interventions based on self-compassion. It found that self-compassion “was found to be a protective factor, in that men with higher self-compassion reported a weaker relationship between masculine norm adherence and help-seeking behaviors.”
Takeaway
The amount of research pointing out that men are at a higher risk of suicide because of self-stigma, societal expectations, and stigma surrounding mental health in general far exceeds the amount of research aimed at suggesting interventions and solutions. Theorization and hypothesis-building are the very first steps, ones which the research world took more than two decades ago. Public health organizations need to begin more robustly targeting the design, implementation, and evaluation of gender-specific programming to make significant progress in reducing suicide rates.
Feature image: Carlos Henrique, The Man Under The Shadow, used under CC BY-ND 2.0 Graph from NCHS Data Brief No. 241, April 2016. Timeline: Madeline Bishop.
If you are having thoughts of suicide, call the National Suicide Prevention Lifeline at 1-800-273-8255 or visit suicidepreventionlifeline.org.