Over 12,000 home health agencies served 5 million disabled and older Americans in 2018. Home health aides help their clients with the tasks of daily living, like eating and showering, as well as with clinical tasks, like taking blood pressure and leading physical therapy exercises. Medicare relies on home health care services because they help patients discharged from the hospital and skilled nursing facilities recover but at a much lower cost. Together, Medicare and Medicaid make up 76% of all home health spending.
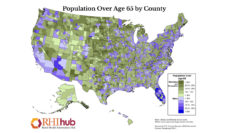
Home health care workers serve a particularly important role in rural areas. As rural areas lose physicians and hospitals, home health agencies often replace primary care providers. The average age of residents living in rural counties is seven years older than in urban counties, and this gap is growing. The need for home health agencies serving the elderly in rural areas will continue to grow over the coming decades.
Rural home health agencies face unique challenges. Low concentrations of people are dispersed over large geographic areas leading to long travel times for workers to drive to clients’ homes. Agencies in rural areas also have difficulties recruiting and maintaining a workforce. Due to these difficulties, agencies may not be able to serve all rural beneficiaries, initiate care on time, or deliver all covered services.
Congress has supported measures to encourage home health agencies to work in rural areas since the 1980s by using rural add-on payments. A rural add-on is a percentage increase on top of per visit and episode-of-care payments. When a home health aide works in a rural county, Medicare pays their home health agency a standard fee plus a rural add-on. With a 5% add-on, Medicare would pay $67.78 for an aide home visit in a city and $71.17 for the same care in a rural area.
Home health care workers serve a particularly important role in rural areas. As rural areas lose physicians and hospitals, home health agencies often replace primary care providers.
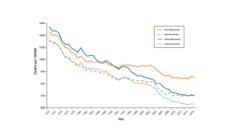
Rural add-on payments have fluctuated based on Congressional budgets and political priorities. From 2003 to 2019, the amount Medicare paid agencies changed eight times. For instance, the add-on dropped from 10% to nothing in April 2003. Then, in April 2004, Congress set the rural add-on to 5%.
The variation in payments created a natural experiment for researchers. Tracy Mroz and colleagues assessed how rural add-ons affected the supply of home health agencies in rural areas. They asked if the number of agencies in urban and rural counties varied depending on the presence and dollar amount of rural add-ons between 2002 and 2018. Though rural add-ons have been in place for over 30 years, researchers had not previously investigated their effect on the availability of home healthcare.
The researchers found that rural areas adjacent to urban areas were not affected by rural add-ons. They had similar supply to urban areas whether or not add-ons were in place. In contrast, isolated rural areas were affected substantially by add-ons. Without add-ons, the number of agencies in isolated rural areas lagged behind those in urban areas. When the add-ons were at least 5%, the availability of home health in isolated rural areas was comparable to urban areas.
In 2020, Congress implemented a system of payment reform that reimburses home health agencies in rural counties by population density and home health use. Under the new system, counties with low population densities and low home health use will receive the greatest rural add-on payments. These payments aim to increase and maintain the availability of care in the most vulnerable rural home health markets. Time will tell if this approach gives sufficient incentive to ensure access to quality care in the nation’s most isolated areas.
Photo via Getty Images