Health care providers and systems are increasingly under pressure to improve the management of chronic conditions while simultaneously reducing costs of care. One chronic condition that has garnered a significant amount of attention is diabetes. This focus is not surprising, as the savings that can result from diabetes prevention are striking. The Centers for Medicare and Medicaid Services (CMS) spends $42 billion more on beneficiaries with diabetes than on non-diabetic beneficiaries. Many clinical interventions are targeting at-risk individuals for increased education and services.
Little attention, however, has been given to improving the food environments of diabetic patients. Management of diabetes is highly dependent on dietary intake. The quantity and quality of foods consumed affect blood glucose levels. Untreated hyperglycemia in diabetics can lead to cardiovascular disease, kidney disease, infection from damaged blood vessels, and emergency complications like diabetic ketoacidosis.
Our analysis suggested that higher ratios of fast food outlets to grocers were significantly associated with higher rates of hospitalizations among diabetics.
As such, individuals with diabetes are encouraged to limit their intake of processed carbohydrates, saturated and trans fatty acids, cholesterol, and sodium. Dietary intake, may be influenced by the local food environment. Some research suggests that food environment characteristics are associated with fruit and vegetable consumption and other dietary quality measures as well as with obesity. These characteristics include distance to and density of neighborhood grocery stores, fast food restaurants, and convenience stores. Poor quality food environments may make adults with diabetes more vulnerable to complications caused by poor dietary intake, placing them at a distinct disadvantage.
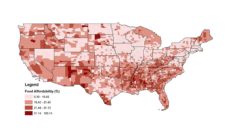
In a recent study we analyzed the association between “food swamps” and hospitalization rates among diabetic adults. Food swamps are areas in which large numbers of unhealthy energy-dense food offerings inundate or “swamp out” healthy food offerings. We measured food swamps using the ratio of fast food outlets to grocery stores in a county.
Our analysis suggested that higher ratios of fast food outlets to grocers were significantly associated with higher rates of hospitalizations among diabetics. Furthermore, this association was stronger in rural counties than in urban counties.
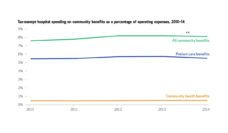
These findings hint that improving food environments may provide an additional opportunity for policymakers and health systems to intervene in diabetes prevention and management. Future efforts to reduce hospital visits among diabetic patients may want to look beyond the clinic and include ways to help patients in food swamps access healthier food. One example of such an effort is Geisinger Health’s Fresh Food “Farmacy,” which provides diabetic patients with meal plans and groceries at the hospital site. These interventions may in fact be quite cost effective. Our findings also support food environment regulations, such as zoning restrictions for fast food outlets, which can improve health outcomes for entire communities.
Photo by Miguel Andrade on Unsplash