Dentist visits can strike fear into the hearts of even the toughest of people. As Johnny Depp once said, “Trips to the dentist…I like to postpone that kind of thing.” While some avoid the scraping and poking by choice, others are kept from their yearly recommended check-ups because of high costs and a lack of insurance. Persons who are low-income, uninsured, and those covered by Medicaid in the United States have dismal oral health outcomes, especially in rural areas.
How important is oral health care, really?
Children with oral health issues have worse attention spans, poor school performance, and a higher likelihood of sleeping and eating disorders. Adults with dental problems face challenges in getting and keeping employment, and maintaining relationships. Diabetes, respiratory issues, heart disease, and stroke have all been linked with poor oral health as well.
Untreated tooth infections have even proven to be fatal. In one case, 12-year-old Deamonte Driver’s mother failed to find a dentist who would accept Medicaid to perform her son’s tooth extraction procedure. Without care, Driver’s toothache became an untreated infection, leading to hospital admission, two expensive brain surgeries, and death. Twenty-four-year-old Kyle Willis delayed dental care due to lack of access when he was unemployed and lacked insurance. He put off a wisdom tooth extraction, which became infected. Unable to afford both the painkillers and the antibiotics that were prescribed to him by the emergency room, he chose the cheaper of the two. Without the antibiotics, the tooth infection spread to his brain. Driver died in 2007, Willis in 2011, both from infected tooth abscesses.
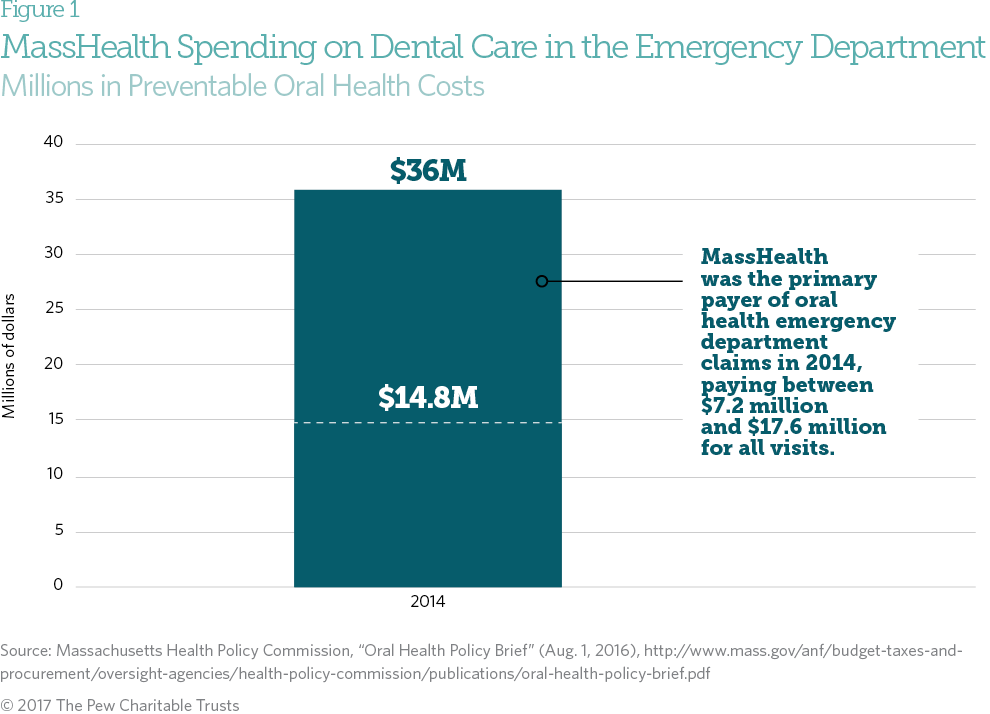
The Massachusetts health care system paid between $15 -$36 million for emergency dental care in 2014. MassHealth – the state’s Medicaid program – alone paid between $7.2 million and $17.6 million. The costs were driven by over 36,000 E.R. visits, many of which were due to untreated, preventable dental crises.
What about dental insurance?
Dental health care and medical care have separate insurance and payment systems. This creates financial burdens for both patients and dentists. Dental plans typically underpay for specialty care and fail to authorize reimbursement for routine dental care. Only 40% of dentists nationwide accept Medicaid, according to the American Dental Association. In some states, Medicaid programs only cover emergency dental care. In others, there is no provision for adult dental care at all.
“It is a common opinion within the dental community that if Medicaid and insurance reimbursements didn’t drive practitioners to lose money on certain procedures, many more would practice in areas where fee-for-service dentistry isn’t the norm,” writes University of Colorado dental student Amanda Hand. “Many dentists believe that more changes to Medicaid and insurance reimbursements need to be made in order to drive practitioners to ‘low-income’ areas.”
What—or who—can fill the gap?
The dental health care system remains afflicted by the “silent epidemic” noted by the U.S. Surgeon General in 2000. Tragic cases like those of Driver and Willis elevated public awareness about the importance of oral health, which was added to the list of twelve Leading Health Indicators of the Healthy People 2020 initiative. Pediatric dental coverage was added to the list of Essential Health Benefits within the Affordable Care Act. But notable access issues remain.
The field of dental therapy has emerged as a promising solution to eliminate oral health disparities. Dental therapists, also known as mid-level providers, receive rigorous training in a more limited scope of care than fully licensed dentists. They provide preventive and restorative treatments like tooth extractions and cavity fillings, generally with substantial oversight from dentists. “We go through the same requirements for testing with the state,” Gina Buchal of Children’s Dental Services in Minneapolis, MN tells NBC News. “Our licensure exam is the same that the DDS [Doctor of Dental Surgery] take, we just take a smaller portion of it.”
As such, they receive about half the pay of traditional dentists, so they are intended for community health programs with more minimal budgets. This allows dentists to expand their practices and treat more patients in underserved communities, schools, and nursing homes.
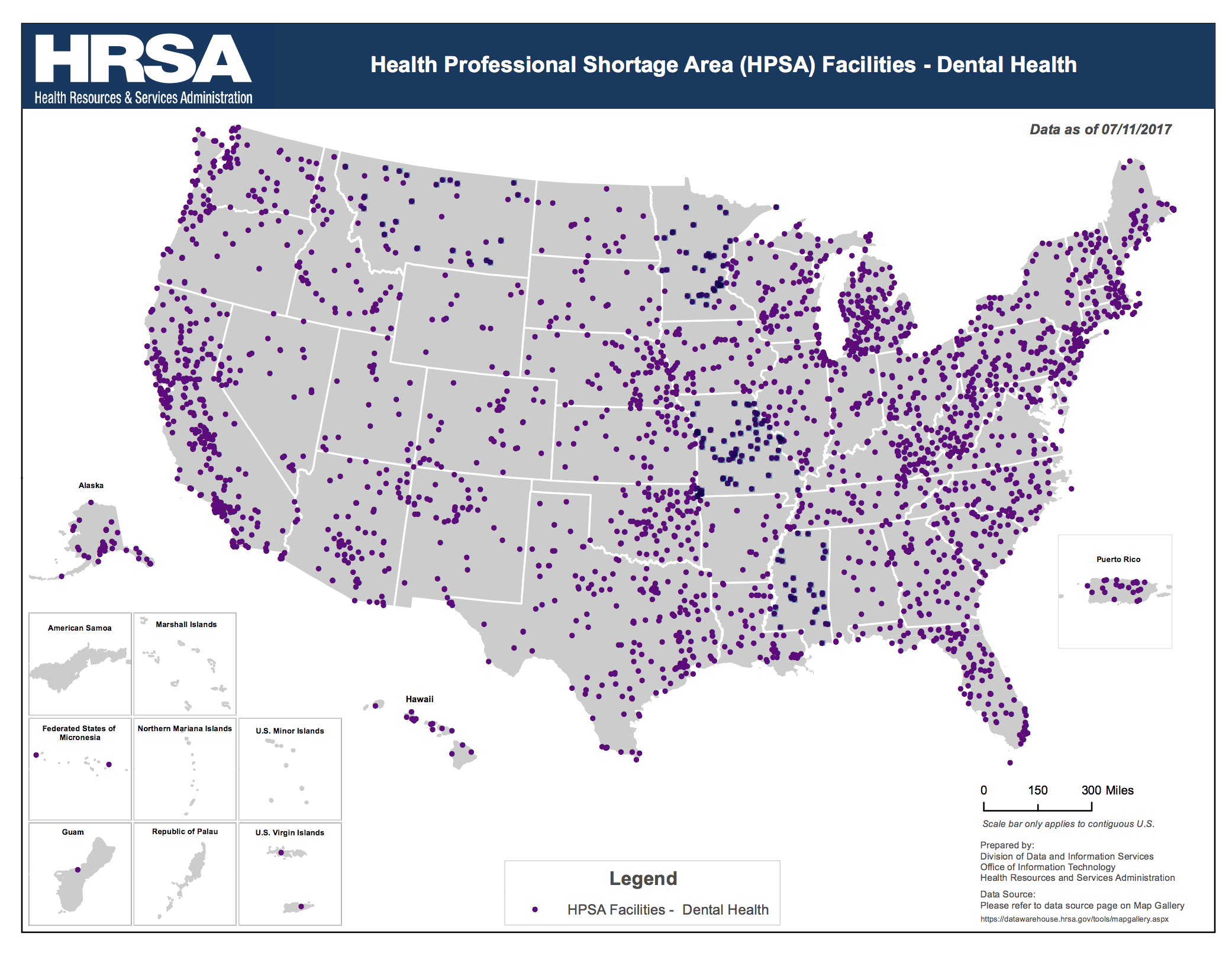
Dental therapy began in the United States in 2004 in Alaskan tribal communities and has been authorized in several states since. Some states like Massachusetts are considering provisions that would authorize dental therapists to practice in counties with dental shortages and treat Medicaid patients. In their March 2017 commentary, researchers Y. Tony Yang, Brian Chen, and Tanya Wanchek explain that even these more limited provisions could bring much needed services to the 10% of Americans who live in areas with limited or no access to dental health providers.
Why the skepticism?
Controversy in the dental community remains a barrier for scaled-up acceptance of dental therapists. Yang, Chen, and Wanchek report that dentists fear competition from lesser-paid counterparts. Dentists also question whether therapists’ widespread use would result in a “discriminatory dental care system,” in which those who can afford it will go to dentists, and those who cannot will get dental care that is less safe or of diminished quality. Yet studies have shown that the presence of dental therapists, both domestically and in the more than 50 other countries where they are used, generally results in a similar quality of care, increased access, less dental disease, and lowered costs.
The states that have authorized the use of dental therapists and those that are considering it have a variety of education and licensing requirements. This patchwork array of standards complicates and hinders scale-up, and perpetuates a lack of understanding amongst dentists and dentists-in-training. Importantly, the United States Commission on Dental Accreditation is beginning to consider uniform standards for dental therapists, which may help to minimize skepticism among dentists and spread the benefits of dental care to areas where dentists have traditionally declined to practice.
Feature image: Partha S. Sahana, a tooth, Indispensable instrument at dental office – Mirror & Probe (Image reflection without editing), used under CC BY 2.0
Graphics: Pew Charitable Trusts, and Health Resources & Services Administration