Imagine someone named David, who sees the “M” listed on their birth certificate. That M indicates they were assigned male at birth, but David knows this to be wrong; David identifies as female.
David decides to seek transition-related care, which helps transgender people to express the gender they knows themselves to be. Specifically, David wants to start hormone therapy. These hormones will lead to changes in David’s physical appearance to match their gender identity. Hormone therapy is associated with improved mental health outcomes, including lower levels of depression and anxiety.
However, David does not have health insurance to cover their transition-related care. They were recently denied a job because they are transgender, leaving them without employer-sponsored insurance. Furthermore, David lives in one of nine states where Medicaid does not cover gender-affirming hormone therapy.
This scenario is common for transgender people, who face numerous challenges when they try to access gender-affirming care. Transgender people are more likely to be uninsured than the general population; employment discrimination is a major cause. According to the National Transgender Discrimination Survey, 26% of transgender and gender non-conforming adults reported losing their job because of their gender identity. And nearly 45% reported receiving no job offers. Furthermore, transgender adults are four times as likely as the general population to be living under the poverty line. This means paying out-of-pocket for health care and private insurance is often out of reach.
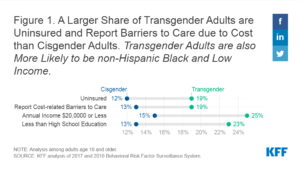 As a result of these barriers, transgender people may forgo hormone therapy altogether, or turn to alternative sources such as purchasing hormones online or from friends. A team from the University of Michigan decided to examine the relationship between insurance coverage and patterns of hormone use among transgender individuals. They used data from the US Transgender Survey collected from August to September 2015.
As a result of these barriers, transgender people may forgo hormone therapy altogether, or turn to alternative sources such as purchasing hormones online or from friends. A team from the University of Michigan decided to examine the relationship between insurance coverage and patterns of hormone use among transgender individuals. They used data from the US Transgender Survey collected from August to September 2015.
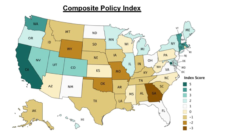
The research team found that transgender people who had insurance were 2.3 times more likely to be using hormones than those who were uninsured. However, 21% of insured individuals still had their claims for hormone therapy denied. Type of insurance matters. Those with Medicaid were more likely to have their hormone therapy claims denied compared to those with private insurance.
While insured transgender people are more likely to use hormones, uninsured transgender people were 2.6 times more likely to use non-prescription hormones. Accessing hormones from unlicensed sources, such as the internet or from friends, may carry additional risks since these hormones are not monitored for content and quality.
However, some transgender people may prefer to access outside sources because of the discrimination and outright denial of care they experience from providers. In fact, 28% of transgender individuals avoid care altogether. Instead, they seek alternative avenues for the transition-related services they need.
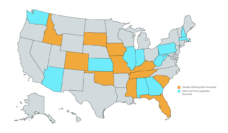
Policy makers and insurers must eliminate barriers to gender-affirming care. Ensuring all transgender individuals have access to affordable health insurance is the first step. More than 55% of US adults receive health insurance through their employer. Eliminating employment discrimination would increase the number of transgender people with insurance. Currently, only 22 states plus DC prohibit discrimination based on both sexual orientation and gender identity.
Expanding Medicaid can also help transgender people get health insurance coverage. Traditional Medicaid excludes most childless adults, which leaves many transgender people in the coverage gap. This means they do not qualify for either Medicaid or premium subsidies. The Biden administration offered additional financial incentives for Medicaid expansion to the 12 states who have not expanded Medicaid. It is unclear whether these states will take the offer.
Getting all transgender people insured is only the first step, as many insurance companies continue to deny claims for gender-affirming care. This occurs despite state and federal laws that make it illegal for health insurance plans to deny coverage for medically necessary transition-related care. Organizations like the National Center for Transgender Equality and Lambda Legal can help transgender people navigate the coverage process to get the care they need.
Photo via Getty Images