Public Health Post: What characteristics of the Covid-19 pandemic had the largest effects on mental health?
M. Daniele Fallin: I am not sure we have the evidence to say what was the largest impact, but data suggest financial hardship was a big contributor, as well as the intersection of the pandemic with racial justice concerns and a contentious election in 2020. Specific to the pandemic, there were fears of infection of self and loved ones as well as grief of life and health lost, but also of experiences lost. There was psychological distress associated with safety measures such as isolation. In times of hardship, we often lean on each other for social and emotional support, but the pandemic forced us to find that support virtually.
Research indicates that the pandemic has posed additional challenges for people battling addiction. What other communities have had increased difficulty adjusting to the pandemic?
As mentioned those most financially impacted by the pandemic, including those who lost their jobs, or who were already at low income levels. Those with chronic conditions, both mental and physical, appeared to experience greater distress. Children were also particularly vulnerable, although data on the short-and long-term impacts is only now being captured or analyzed. Interestingly, emerging adults were highly impacted compared to other adult age groups, at least early on. This time of life is in general a sensitive time in terms of emerging psychopathology, with first onset of mental illness often occurring in this window.
How do the mental health impacts of Covid-19 compare to those of the September 11 attacks?
The differences between effects of natural disasters and other traumatic events such as 9/11 are hard to extrapolate to the Covid-19 experience for a variety of reasons. First, this was a global event, not isolated to a particular region of the world or country. Second, it was not a single event, but rather a circular evolution of wave, recovery, new wave, recovery, etc. and the waves were not consistent across locations in the US or across the world. We have never had this type of continuing event at this scale to compare to.
Discrimination against certain segments of the population is one of the most pertinent commonalities between the two events. After 9/11, Middle Eastern and Muslim people both experienced increased discrimination in the United States. Similarly, Asian Americans, particularly Chinese Americans, experienced increased discrimination and harm during the Covid-19 pandemic. These populations may have additional stressors that are worth considering when looking at targeted mental health services and programs.
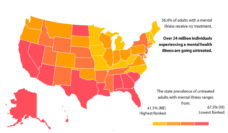
Both inpatient and outpatient mental health treatment services often have long waitlists, something that was further exacerbated by the pandemic. What can we do to make more services available so those who need them can be treated?
Two efforts during the pandemic may be illustrative. First, there was a huge and rapid expansion of telemental health services. Second, for persons with opioid use disorder there was relaxation of methadone prescription requirements, allowing people to take home a longer supply, rather than having to report to a clinic every day. Both of these adjustments expanded access to care and some data has shown that patients have fewer negative outcomes than predicted. Beyond these two examples, there are many other policy and guideline changes we could make to improve access and utilization. They include changes in the workforce infrastructure – who can provide care and be reimbursed, changes in models of delivery – collaborative care for example, and perhaps most importantly, cultural change in acceptance of mental illness and awareness that these conditions are preventable and treatable.
What did we learn about mental health during the Covid-19 pandemic that we should continue to monitor as we near the end?
We learned that narratives matter and that personal connection, either in one’s own experience or the experience of a close friend or family member, are powerful tools for de-stigmatization. Nearly everyone experienced some form of psychological distress during the pandemic, from mild distress to very serious illness. Many for the first time. I have seen that experience and awareness change attitudes among leaders, managers, peers, and family members about the “legitimacy” of mental distress, the need to address it, and a new willingness to be part of a solution. I hope that continues for many years. It would be a huge advance for health in our society.
M. Daniele Fallin will participate in the public health conversation The Next Normal: Mental Health on Tuesday, Nov. 16 at 4:30 p.m. Register here.
Photo provided by M. Daniele Fallin