Public Health Post sat down with Karen deSalvo at the symposium Building Healthy Cities: Boston and Beyond, at the Boston University School of Public Health, which brought together leaders in health to explore approaches for creating healthier cities.
On how her background informed her work at the U.S. Department of Health and Human Services (HHS)
KD: I have a relatively unusual background for someone who is in senior leadership in government. I come from a very poor family, my dad left when I was little so I was raised by a single parent. I put myself through college. I didn’t go to a fancy college, I went to a working-class college… and scrappy, I think, and southern. And there aren’t a lot of people who get through that gauntlet and end up in the Humphrey building. I’m thankful for all the opportunities that I had, but I also made sure that when I was at the table, I was lifting up the voice of the people who grew up on my street when I was a kid. I wanted to make sure that it wasn’t just a limited view on the world and the people we’re there to serve.
I tried to make sure that every day, my work as a doctor, my work as a community advocate, and my work as the health commissioner was in my heart and mind in the work that I did. And some of the technique as a health commissioner in particular, learned from that mayor, I carried with me to HHS. Listening sessions and community engagement being a big part of that.
On Washington leadership and public health
I think the reality is that most, if not, nearly all health policy people and national health leaders in Washington do not know what public health is. And I got to the point towards the end of my tenure that I was probing, asking people questions just to see what kind of answer I get. And you invariably get an answer about public hospitals and Medicaid and community health centers, which is problematic because the Secretary of Health and Human Services has at their disposal an enormous array of tools that can impact health.
I think the reality is that most, if not, nearly all health policy people and national health leaders in Washington do not know what public health is.
So, I think there’s an opportunity there once people understand it. But the truth is when you’re in the seat of Secretary, you spend a lot of time thinking about the ACA. Or now in this world, the ACA and the AHCA, and the responsibilities of running a federal marketplace, which is poorly funded so requires a lot of rolled up sleeves.
Even as important as the CDC and the NIH and the FDA are in their various public health roles and the communicable disease work that is often at the forefront for the Secretary, the other kinds of public health work, the systemic, policy level change doesn’t always get the kind of attention…so, we have a lot of work to do. One of the last things I did was form a social determinants of health work group, I don’t know if it’s still in existence. We set a very high level work plan.
On the importance of qualitative research
It’s really easy when you get in that bubble at HHS—that big concrete building—to lose touch with people’s voices in the real world. And the kind of people that come see you, there are lobbyists or people who are fancy and you could go to work every day as a policymaker for the people of this country and not even ever see poverty. And so, the idea that—and big data doesn’t help get you to that, it’s cold and disconnected—but qualitative research is real, it’s a touchstone. And the stories and what you gain from the kind of the assembly of all the stories into some shared themes.
On her work with social determinants of health
What the inclination for your staff to do is to invite people that they know will tell you what you’re doing is great. And that’s not exactly…what I don’t need to hear. I need people to tell me what we’re doing is not great, or how it’s not helping. That’s the valuable conversation,
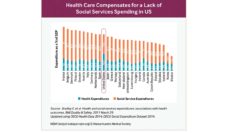
I was annoying about the social determinants all the time, everywhere I could be. And about the importance of not letting the health care system crowd out the public health and social services infrastructure in this country, which has deep and tight connections with community and people and that we need to support them.
On the business case for addressing social determinants of health
Well, I think the near-term business case mostly has to be focused on health care costs, for lots of reasons. One it’s a focal point of attention, it’s a sixth of the economy. There’s a lot of waste in the system; there’s a lot of opportunity to save 750 billion dollars a year and reinvest that upstream in other determinants if we could sort out the ways to do that. So, there’s a lot to be gained if it’s done right.
I think where the best business case can be made right now, where it’s not just a nice-y nice idea, is for payers who are highly at risk, like Medicaid managed care organizations or Medicare Advantage, where they are asking for this kind of resource. The health systems that are both a payer and a provider are also—because they are more at risk—they are also quite interested in understanding social factors. And governors, they make a strong business case because every dollar they have to spend on a Medicaid program because of unmet social needs is a dollar they can’t spend on the educational system. So those are constituencies that are paying a lot of attention.
Feature image: Dr. Karen DeSalvo (middle) with Dr. Karen Murphy, Secretary, Pennsylvania Department of Health (left) and Dr. Karen Hacker, Director, Allegheny County Health Department (right). Photo courtesy Karen DeSalvo.