At the emergency room, most of us will not think about whether the doctor treating us is in our insurance network. And yet, each year, millions of Americans receive a surprise–and often, very pricey–bill from the doctor whom we “chose” only because we had shown up in her emergency room and who, it turns out, does not accept our insurance coverage. Known as balance billing, these charges can be confusing and upsetting. Unexpectedly, we have to pay out of our pockets for care we thought was covered.
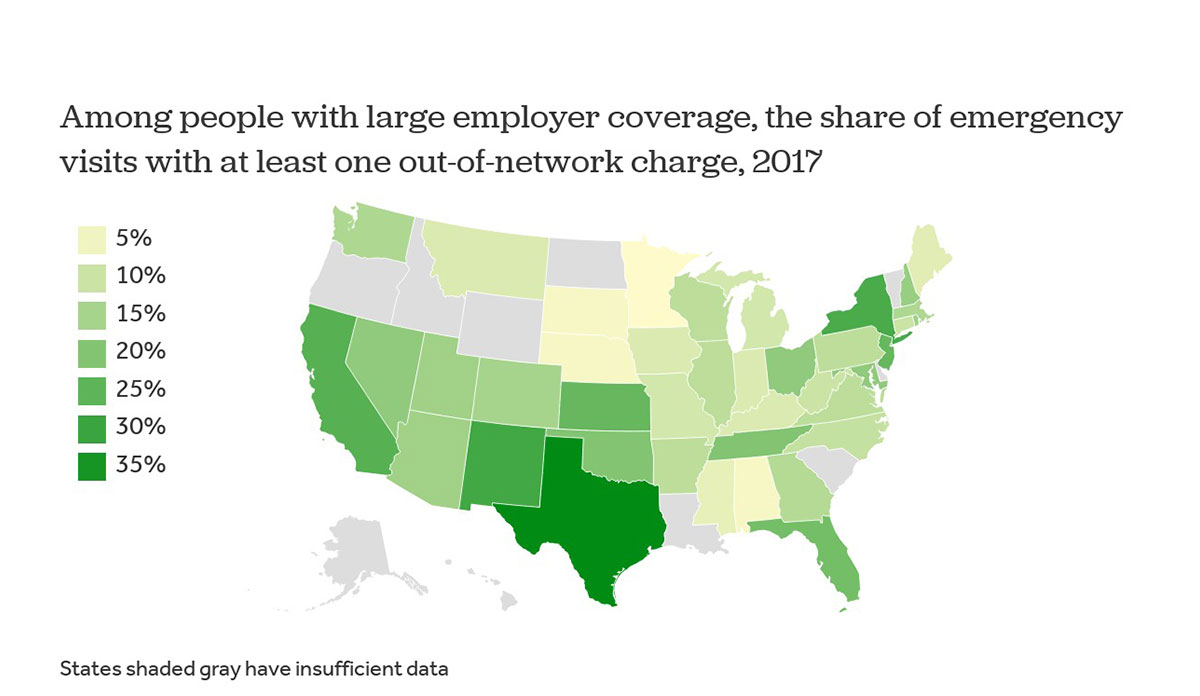
New analysis from the Peterson-Kaiser Health System Tracker looked at these surprise bills in the context of emergency care. Using data from large employer health plans in all 50 states, Peterson-Kaiser found that nearly 20% of all ER visits resulted in a surprise bill.
States varied in the proportion of visits resulting in an out-of-network charge. In Texas and New York, the rates are as high as 38% and 28%, respectively. In other states, such as Minnesota and Nebraska, patients experienced a surprise bill in only 2% of visits. This range may be explained by different state-level policy solutions, which include standard payment rates and formal arbitration hearings.
The ongoing national healthcare debate typically focuses on expanding access to the uninsured. However, surprise bills are delivered to fully insured patients. Given that four-in-ten Americans would struggle to pay an unexpected expense of $400, Congress needs to address this critical deficiency. These bills are typically far more expensive than just $400, putting too many seemingly health-insured Americans into debt.
Databyte via An Examination of Surprise Medical Bills and Proposals to Protect Consumers from Them. Peterson-Kaiser Health System Tracker, 2019.