Frontline health care workers and first responders have experienced many stressors during the COVID-19 pandemic. They’ve feared for their safety and that of their close contacts. They have been separated from family and exposed to a million deaths, waves of suffering, and have experienced prolonged periods of exhaustion.
Rebecca Hendrickson and her research team investigated the factors driving health care workers and first responders to leave their jobs. They surveyed 710 people about their COVID-19-related occupational stressors and how well they were performing at work. The questions focused on symptoms of depression, anxiety, insomnia, and post-traumatic stress disorder (PTSD).
Workers who reported higher occupational stressor levels were more likely to show symptoms for all psychiatric conditions than colleagues with fewer stressors. Health care staff reported having trouble doing their usual work. Half said they were more likely to quit their jobs because of the pandemic.
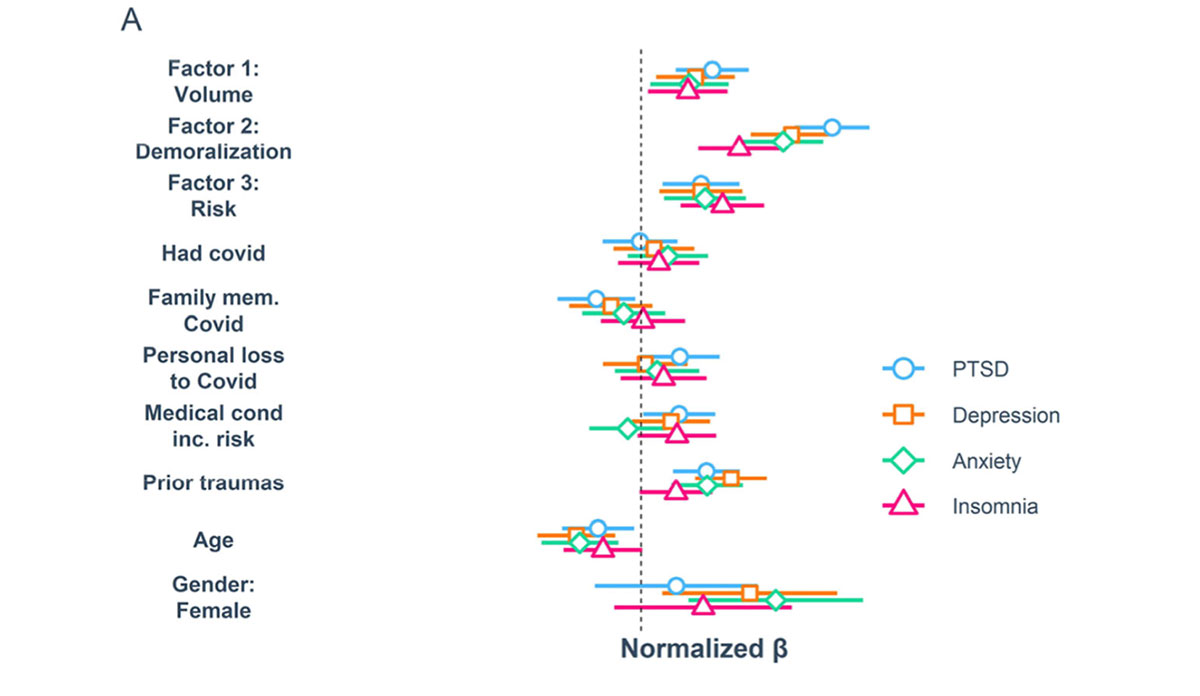
The figure shows the association between various occupational stressors and the four psychiatric symptom categories, represented by the colorful shapes. Almost all risk factors—most notably volume of COVID-19 patients cared for and perceived risk of infection– were positively associated with the psychiatric symptoms measured.
A notable theme that emerged from a “write-in” option was that many workers felt “betrayed” by low community vaccination rates. Demoralization (defined as perceived inadequate support or feeling ineffective) showed strong associations with symptoms of all four psychiatric conditions. Such symptoms have been associated with disinvestment in patient care, which can be a risk factor for family members of hospitalized patients developing PTSD themselves.
The authors recommend that hospitals reduce unnecessary workload and find means to enhance frontline worker input within workplaces. Workforce sustainment strategies might include providing more childcare to workers during school closures, providing additional formal mentorship or peer support structures for younger hospital staff, and proactively encouraging employees to seek supportive care for personal distress.
When health care workers feel supported, everyone benefits.
Databyte via Rebecca C Hendrickson et al. The Impact of the COVID-19 Pandemic on Mental Health, Occupational Functioning, and Professional Retention Among Health Care Workers and First Responders. Journal of General Internal Medicine, 2022.