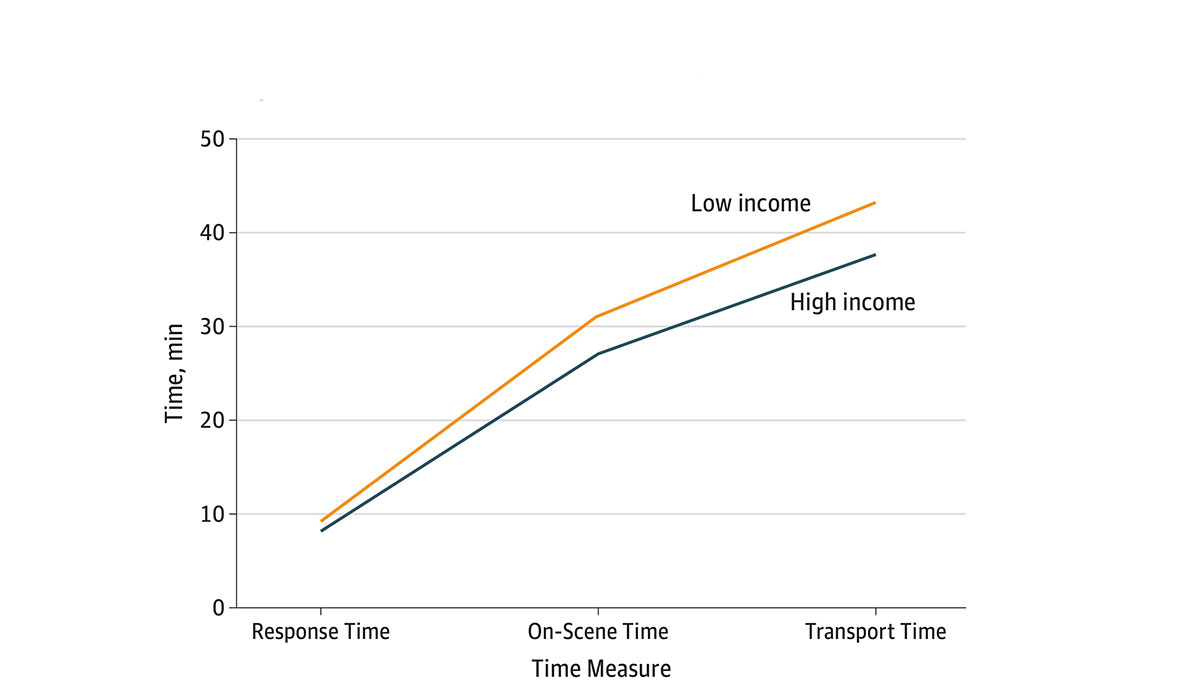
How long do you think it takes for an ambulance to respond to a 9-1-1 call and get a patient to a hospital? In a recent study, Renee Y. Hsia and colleagues assessed 63,000 cardiac arrest EMS encounters to determine whether ambulance response times were longer in low-income versus high-income urban zip codes. The graph above displays three measures, comparing low-income and high-income neighborhoods: 1) the time in minutes between EMS dispatch to arrival at the patient’s location (Response Time), 2) the time between EMS arrival and departure (On-Scene Time), and 3) the time between scene departure and arrival at the destination hospital (Transport Time).
The total EMS time (Response + On-Scene +Transport) for low-income communities was 3.8 minutes (10%) longer than in high-income neighborhoods. The gap in time between the two areas is largely attributable to On-Scene Time, which was 2.8 minutes (15%) longer in low-income zip codes. The authors do not give insight as to why on-scene time has the biggest gap in time, but possible barriers impeding immediate care from EMTs in low-income neighborhoods might include congested streets, narrow doorways, and buildings without elevators. The authors cite several additional barriers such as scene safety and distance from a hospital that may have contributed to the differences in total time.
This study is one of the first to document delays in EMS care by zip code. Although a few minutes may not appear to be an important difference, survival or death may be determined in a matter of minutes. The authors note that cardiac care delayed by just one to four minutes has been associated with increased mortality.
Databyte via Renee Y. Hsia, Delphine Huang, Clay Mann, and et al., A US National Study of the Association Between Income and Ambulance Response Time in Cardiac Arrest. JAMA Network.