Supervised injection facilities (SIFs) are increasingly being discussed in the United States as a way to reduce overdose deaths in the opioid epidemic. Here’s the first article in our week-long debate on SIFs as a harm reduction strategy. Read part two and three here.
On April 29, 2017, the Massachusetts Medical Society endorsed the legalization of supervised injection facilities. I am the sponsor of a bill to create a framework for legal operation of these facilities. The bill is a conversation starter—it needs a lot of refinement as piece of legislation. But the bill speaks to a crying need, now that fentanyl is on the market being sold as heroin.
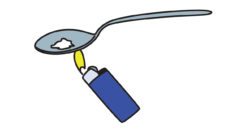
Supervised injection facilities bear no resemblance to the chaotic shooting galleries where people die in the dark, slouched against bare brick. They are quasi-medical clinics where people check-in and then enter an adequately lit individual alcove and, while visible to trained professionals, self-administer the chemicals they have purchased elsewhere. Once it appears that they are not dying of an overdose, they can leave or go to a quiet place.
The facilities offer a unique opportunity to offer drug treatment and AIDS counseling. Properly run, supervised injection facilities can be a tool, not only for reducing the harms of addiction, but also for fighting addiction itself.
Injecting a chemical one bought on a street corner into one’s blood—there are few more terrifying thoughts for most of us.
Yet thousands of people in Massachusetts do exactly that every day—many of them with enough education to know that they are taking wild risks every single time that they do it: risks of infection, risks of poisoning, risks of deaths from overdose. Even as obvious signs of harm emerge—ugly infected abscesses at the spot of injection, friends dying around them—they continue.
Most people with opiate substance use disorders need medically-assisted treatment and huge ongoing support to have a shot at recovery.
That is the essence of the disease: seeking pleasure or relief from compulsive need with denial of—absolute emotional blindness to—emerging harms. Supervised injection facilities are a harm reduction strategy.
Harm reduction strategies are sickening to consider, because they mean accepting the reality of substance use disorder as a chronic relapsing disease—something that people don’t recover from because we tell them to, something that people don’t recover from despite their firmest personal resolutions, something that people don’t recover from even if we punish them for it. Most people with opiate substance use disorders need medically-assisted treatment and huge ongoing support to have a shot at recovery.
Over the past five years, the death rate from overdose has tripled in Massachusetts. While opiate addiction has been spreading and is now tragically endemic among people of all ages, the death rate appears to be growing much faster than addiction.
With fentanyl rampant, we need supervised injection facilities more than ever.
Fentanyl is one of a family of highly potent chemicals which, in microscopic doses, feel like heroin and are now widely available on the blackmarket, often sold as heroin. Because they are so potent, they are heavily mixed with inert substances before sale. Mixes prepared by amateurs will inevitably be uneven—some doses from the mixture will be much more potent than others.
As reckless as they are, many addicts use some caution in the injection process and have a sense of their own tolerance and limits. With fentanyl though, they have no idea of what they are doing to themselves and that is why fentanyl is now the most frequently identified chemical in overdose deaths. With fentanyl rampant, we need supervised injection facilities more than ever.
The real political challenge for creation of a supervised injection facility is finding the private and municipal leadership to create one. In Vancouver, where they have a very well-studied SIF, the political conditions may have been rather unique—there is a neighborhood with a very high concentration of drug users who organized themselves politically. In Massachusetts, it remains to be seen whether we have a neighborhood that is willing to host such a facility.
Until we have a concrete, professional proposal for a facility and the support of local officials, it will be hard for the legislature to focus on my proposed legislation.
Feature image: Insite, the first legal supervised injection site in North America. Photo courtesy Vancouver Coastal Health.
Originally published by Will Brownsberger, on May 3rd, 2017.