Editors note: This article was updated May 5, 2017 referencing the AHCA’s passage in the House] Even with the first vote in the U.S. House on Thursday, May 4th, ACA repeal still looks unlikely. The reason? Moderate and conservative Republicans cannot agree on whether to slash taxes and coverage or to trim and temper them. Even if the House Republican’s bill were to be enacted in 2017, the reaction to creating 18-24 million more uninsured will soon force Republicans and Democrats to consider a true compromise designed to improve the ACA and set it into a bipartisan context.
The ACA’s structural problems, including its relative unpopularity, deserve attention. Is there a substantive way to fix them with some good Republican ideas? Yes, here are a few of them. If congressional Republicans ever decide to improve, not destroy, the ACA, they might consider something like this.
Stabilize and Grow the Market
The core element of this proposal is an alternative to the ACA’s method for making coverage affordable. The ACA tries to do so via a complex formula for tax credits that depends on projecting a household’s precise income next year – which is literally impossible to do with any credibility – so that eligible applicants pay a progressively scaled percentage of their income toward the second lowest cost silver plan (SLCSP).
Let’s borrow from recent Republican legislation, instead, but with one crucial modification: below, say, 300% of the federal poverty level (FPL), all eligible subscribers get advance premium tax credits (APTCs) amounting to 100% of the full premium of the most basic benchmark plan available to them i.e., the lowest-priced bronze plan in their zip code. Here is a simple, bronze, high-deductible health plan (HDHP) that might serve as this national benchmark plan:
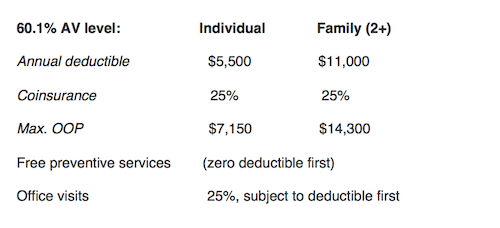 The premium for the lowest cost bronze plan – 85% of SLCSP – should slightly exceed the today’s average APTC for a household between 100% and 300% FPL, so this proposal may increase tax costs per enrollee. Beyond 300% FPL, which approximates median U.S. income, APTCs would phase out in large steps, such as 2/3rds of the full credit from 301-400% FPL, and 1/3rd the full credit from 401-500% FPL.
The premium for the lowest cost bronze plan – 85% of SLCSP – should slightly exceed the today’s average APTC for a household between 100% and 300% FPL, so this proposal may increase tax costs per enrollee. Beyond 300% FPL, which approximates median U.S. income, APTCs would phase out in large steps, such as 2/3rds of the full credit from 301-400% FPL, and 1/3rd the full credit from 401-500% FPL.
The focus on HDHPs is right out of the Republican playbook. However, I propose APTCs that would make the benchmark plan “free” for most of the uninsured. This offers three advantages:
1. “Free” is the most powerful word in sales, and most of the uninsured should opt for coverage;
2. It works reasonably well even without the individual mandate, thereby undercutting much of the popular opposition to the ACA; and
3. Having a free plan makes auto-assignment practical, so that when the uninsured apply for other welfare benefits or fail to renew coverage, they can be auto-assigned.
However, even free catastrophic coverage does not provide access for low-income households. So, I propose to fund the deductible via advance tax credits deposited in the taxpayer’s Health Reimbursement Arrangement (HRA). A reasonable funding level for those below 300% FPL might be the full deductible on the benchmark bronze design. This means that care is essentially free for them while the deductible applies, and then they are responsible for 25% until the out-of-pocket maximum applies. From 300% to 400% FPL, HRA funding might equal half the deductible. Unused funds would revert to the IRS. But unlike the current CSRs, the HRA can bear a certain degree of retroactive funding, which is very helpful when administering credits tied to a household’s projected MAGI. This feature allows HRA funding to be tied directly into tax filings, including real MAGI calculation, for the plan year.
Finally, without an individual mandate, we need to encourage the maintenance of coverage and protection of the risk pool from those who jump in when they need services. Even if free to those below 300% FPL, those above 500% would pay full premiums. There are several ways to protect the risk pool from this sort of adverse selection, without a mandate. I prefer a conventional, commercial underwriting approach: a 6-month waiting period for covering pre-existing conditions for those who have not maintained continuous coverage.
De-regulate ACA marketplaces
Like it or not, ACA supporters are necessarily “in bed with” private health plans: marketplaces depend upon their active participation – not just to enroll people, but to compete on price, network, service, etc.. So, let’s reduce all but necessary requirements on health plans that offer products in the direct market: one standard bronze plan (the benchmark plan) would have to be offered by any issuer that intends to offer health plans that qualify for a tax credit. Beyond that, tax-credit eligible issuers should be required to offer consumers a choice of richer benefits, but of their own design.
Increase Enrollment
The ACA still falls short of its primary goal, to cover 95% of Americans. Why? Because some states have not expanded Medicaid eligibility, as originally modeled, and too many uninsured between 200% and 500% FPL prefer going bare to paying substantial premiums.
Since expanding Medicaid eligibility to 138% FPL has not attracted voluntary participation by 19 states, let’s lower the bar. Why not let the remaining states choose to expand eligibility to 100% FPL, or cap the higher federal funding for all states at 100% FPL? With bipartisan reform, most of the holdout states are likely to raise their income-eligibility standard to 100% FPL, thereby rapidly boosting enrollment and filling in the awkward hole between those who earn too much for Medicaid and too little for APTCs. This one change would reduce the number of uninsured Americans by millions!
Second, one of the advantages of a zero-premium benchmark plan is that it virtually sells itself, even without a mandate. However, we can go even further. We should make auto-assignment to the “zero-premium” benchmark plan the default option, and force eligible tax-filers to make a choice if they prefer to go bare. The ACA now covers only about 60% of APTC-eligible uninsured Americans. The combination of zero-premium coverage and auto-assignment might prove so powerful that we will cover many more uninsured without the individual mandate than with it!
Feature image: Michelle Tribe, broken, used under CC BY 2.0/cropped from original