When public health works, no one sees it – a truth that I’m quite proud of, but also one that creates significant challenges when public health needs support (which is all the time). Evidence of a successful public health program is when people are not getting sick, but unfortunately, decision-makers often notice only when people are getting sick.
This is our challenge as we try to save the Centers for Disease Control and Prevention (CDC)-managed Epidemiology and Laboratory Capacity for Infectious Diseases (ELC) program, a source of crosscutting support for public health laboratories funded under the Affordable Care Act (ACA) through the Prevention and Public Health Fund (PPHF). The PPHF is the first and only mandatory public health funding program in the United States.
ELC is the bedrock of America’s public health detection system. It strengthens epidemiology capacity, laboratory capacity and health information systems (aka, health IT) in 65 local, state and territorial epidemiology and laboratory programs. APHL members – local, state and territorial laboratories – rely on ELC to maintain capacity to effectively and rapidly protect the public’s health. But as President Trump and members of Congress work to repeal the ACA with a focus on the healthcare component, ELC is at risk of repeal without replacement too.
Here’s a quick primer on how ELC works (it’s rather complicated even for those of us immersed in it). ELC has two components. The first is a crosscutting base program which supports basic epi, lab and health IT functions. This is the section that’s included in the PPHF and ACA, and is at risk of being eliminated. It includes support for staff liaisons between laboratory and epidemiology programs, courier systems for transporting potentially hazardous samples and materials, lab equipment and maintenance contracts, scientists who can work across various areas of a laboratory, electronic lab reporting and other crosscutting activities. The second component of the ELC, which does not reside in the ACA, funds response to specific infectious diseases such as Zika, influenza, antimicrobial resistance and foodborne diseases. While this, too, is a critical public health program, its place outside of the ACA means it is safe for now so APHL is focusing efforts on saving the first component.
The public needed this testing far sooner than Congress approved to fund it. Until supplemental funding arrived, public health laboratories could rely on ELC funding to begin their surge testing and response.
What does ELC really mean for public health? How has ELC proven itself invaluable? When it first became clear that Zika posed a significant threat to our country, APHL collaborated with federal partners to expedite implementation of public health laboratory testing. Laboratories needed proper equipment, scientists with the expertise to operate the equipment, systems for receiving samples, systems for communicating results and more.
These are activities that would be covered by designated Zika funding once approved by Congress and distributed by CDC, but, as you may remember, that took about nine months which is a very long time. Public health labs couldn’t wait for the money – they needed to begin surge testing as the number of samples steadily increased. Each of those samples was from an individual desperate to know if they had Zika. In many cases, the individuals were pregnant women and their partners who were concerned for their baby’s health.
The public needed this testing far sooner than Congress approved to fund it. Until supplemental funding arrived, public health laboratories could rely on ELC funding to begin their surge testing and response. Without that funding, the labs – already short on funding for routine testing operations, much less an unexpected outbreak – would not have been able to test the thousands of samples arriving at their doors.
To be very honest, without ELC, I’m not sure what will happen when the weather warms and Zika returns to the US.
I know with certainty that laboratory staff have the expertise and passion to respond, but they are only human. To be very honest, without ELC, I’m not sure what will happen when the weather warms and Zika returns to the US. How will public health laboratories respond effectively to a new threat while still managing routine testing for infectious and foodborne diseases? ELC has allowed public health laboratory staff to jump into action and provided them with necessary support. Without it? I just don’t know.
It’s unfortunate that politics can get in the way of committed epidemiologists and laboratory scientists doing their jobs to protect the public’s health, but it seems to happen often. The frustrating irony of this debate over ACA and concerns over rising health insurance costs is that disease prevention cuts healthcare costs across the board. If people don’t get sick, they don’t miss work, they don’t see their doctors and they don’t go to the hospital. Disease prevention saves money. Yet this deeply political and divisive debate over the ACA has not included mention of the ELC.
If you are interested in supporting the #SaveELC effort, contact your elected officials to remind them that ELC is part of the ACA and to emphasize its value. Encourage them to support keeping ELC intact or, should the ACA be repealed, support an equally impactful replacement. Losing this program will be detrimental to infectious disease detection and response, which could jeopardize the public’s health. Here is additional information on ELC that might be helpful to share. Contact your US Senators, Representative, and President Trump.
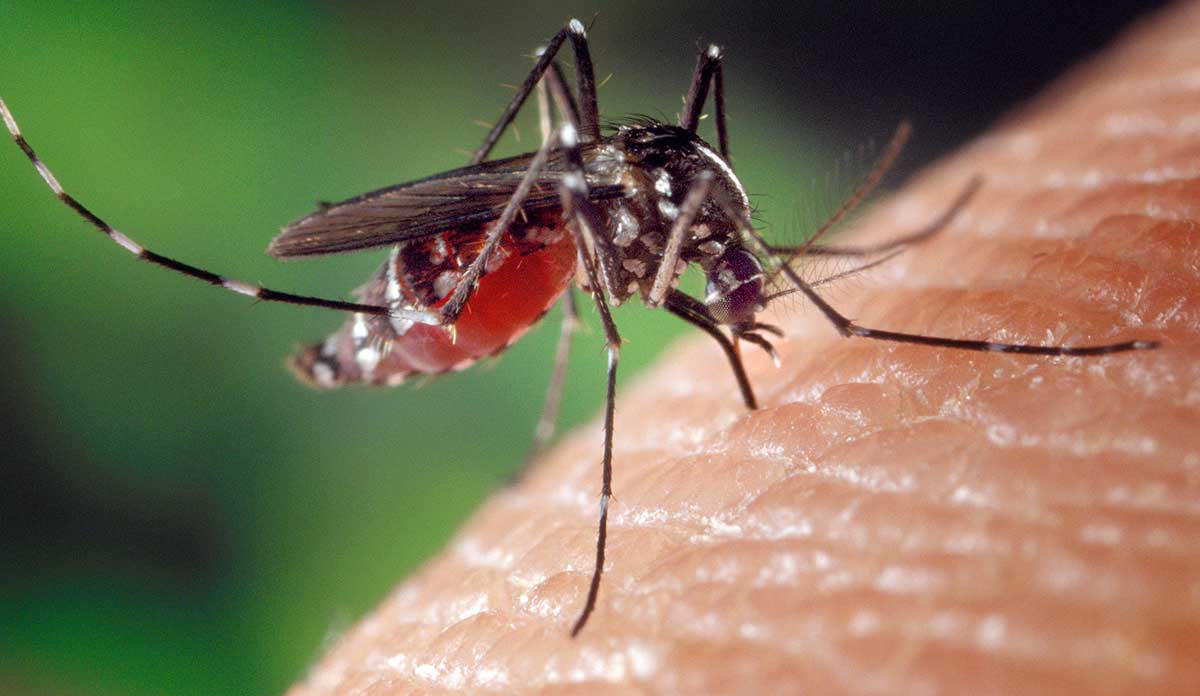
Feature image: CDC Global, A blood-engorged female Aedes albopictus mosquito feeding on a human host. More information on the Zika virus. Used under CC BY 2.0/cropped from original.